Fracture Nomenclature for Thumb Distal Phalanx Fracture
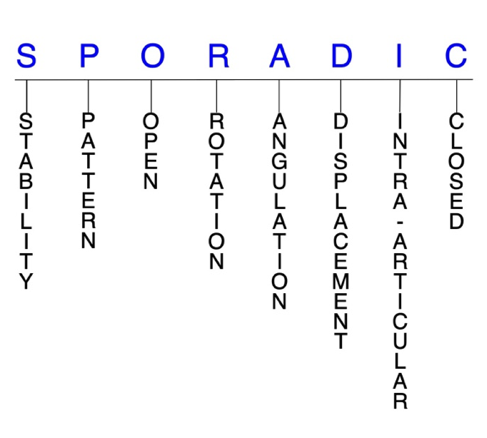
Hand Surgery Resource’s Diagnostic Guides describe fractures by the anatomical name of the fractured bone and then characterize the fracture by the Acronym:
In addition, anatomically named fractures are often also identified by specific eponyms or other special features.
For the Thumb Distal Phalanx Fracture, the historical and specifically named fractures include:
Mallet thumb fracture
IP joint fracture-dislocation
By selecting the name (diagnosis), you will be linked to the introduction section of this Diagnostic Guide dedicated to the selected fracture eponym.
Fractures of the distal phalanx are the most common fractures that occur in the hand, and the thumb is the second most frequently affected digit of these fractures behind the long finger. Thumb distal phalanx fractures are particularly prevalent in sports and work-related accidents, with trauma and crushing forces being the most typical mechanisms of injury.1-4
Definitions
- A thumb distal phalanx fracture is a disruption of the mechanical integrity of the most distal bone of the thumb underlying the nail.
- A thumb distal phalanx fracture produces a discontinuity in the distal phalanx contours that can be complete or incomplete.
- A thumb distal phalanx fracture is caused by a direct force that exceeds the breaking point of the bone.
Hand Surgery Resource’s Fracture Description and Characterization Acronym
SPORADIC
S – Stability; P – Pattern; O – Open; R – Rotation; A – Angulation; D – Displacement; I – Intra-articular; C – Closed
S - Stability (stable or unstable)
- Universally accepted definitions of clinical fracture stability is not well defined in the hand surgery literature.5-7
- Stable: fracture fragment pattern is generally nondisplaced or minimally displaced. It does not require reduction, and the fracture fragments’ alignment is maintained with simple splinting. However, most definitions define a stable fracture as one that will maintain anatomical alignment after a simple closed reduction and splinting. Some authors add that stable fractures remain aligned, even when adjacent joints are put to a partial range of motion (ROM).
- Unstable: fracture fragments will not remain anatomically or nearly anatomically aligned after a successful closed reduction and simple splinting. Typically unstable thumb distal phalanx fractures have significant deformity with comminution, displacement, angulation, and/or shortening.
P - Pattern
- Thumb distal phalanx tuft: oblique, transverse, or comminuted; tuft fractures usually result from crush injuries, and they are often comminuted and nearly always associated with an injury to the nailbed matrix, digit pulp, or both.1,8
- Thumb distal phalanx shaft: transverse, oblique, or comminuted with or without shortening; transverse shaft fractures are potentially unstable, as the fracture angulates with its apex anterior secondary to the pull of the flexor pollicis longus (FPL) tendon on the proximal fragment.1
- Thumb distal phalanx base: can involve the interphalangeal (IP) joint; these intra-articular fractures usually involve the dorsal or volar lip of the thumb distal phalanx base.
O - Open
- Open: a wound connects the external environment to the fracture site. The wound provides a pathway for bacteria to reach and infect the fracture site. As a result, there is always a risk in developing osteomyelitis. Therefore, open fractures of the thumb distal phalanx require antibiotics with surgical irrigation and wound debridement.5,9,10
R - Rotation
- Thumb distal phalanx fracture deformity can be caused by proximal rotation of the fracture fragment in relation to the distal fracture fragment.
- Degree of malrotation of the fracture fragments can be used to describe the fracture deformity; this is not a common type of fracture deformity in the thumb distal phalanx.
A - Angulation (fracture fragments in relationship to one another)
- Angulation is measured in degrees after identifying the direction of the apex of the angulation.
- Straight: no angulatory deformity
- Angulated: bent at the fracture site
- Example: thumb distal phalanx fractures with >20-30° of angulation in the sagittal plane can result in extensor lag of the IP joint1
D - Displacement (Contour)
- Displaced: disrupted cortical contours (eg, thumb distal phalanx shaft fractures can be displaced or translated partially or completely)
- Nondisplaced: fracture line defining one or several fracture fragments; however, the external cortical contours are not significantly disrupted
I - Intra-articular involvement
- Fractures that enter a joint with one or more of their fracture lines. Intra-articular fractures of the thumb distal phalanx require special attention due to the digit’s indispensible role in hand function.10
- Thumb distal phalanx fractures can have fragment involvement with the IP joint.
- If a fracture line enters a joint but does not displace the articular surface of the joint, then the risk of developing post traumatic osteoarthritis is relatively low. If the articular surface is separated or there is a step-off in the articular surface then the congruity of the joint will be compromised and the risk of posttraumatic osteoarthritis increases significantly.
C - Closed
- Closed: no associated wounds; the external environment has no connection to the fracture site or any of the fracture fragments.5-7
Thumb distal phalanx fractures: named fractures, fractures with eponyms and other special fractures
Mallet thumb fracture
- An avulsion fracture of the extensor pollicis longus (EPL) tendon from its distal phalangeal insertion at the dorsal base of the bone is commonly referred to as mallet thumb.1,11
- Results from a flexion force directed to an actively extended thumb, which hyperflexes the IP joint and produces either stretching or tearing of the extensor tendon substance or an avulsion of the tendon from its insertion on the distal phalanx.12
- Most occur in a work environment or during sports participation.8,12
- Mallet thumb is far less common than mallet finger, accounting for ~2-3% of all mallet injuries. Thus, less is known about mallet thumb.13
- In one study, individuals with mallet thumb had a smaller percentage of fragment displacement and articular involvement, as well as no subluxation, compared to those with mallet finger injuries. This may be due to greater extensor strength of the EPL compared with the terminal extensor tendon, differences in the tendon attachments, and tighter capsule that together make the IP joint more stable and limit subluxation.
- Patients also presented earlier than those with mallet finger, which may be due to the relative importance of the thumb to hand function and the fact that the extensor lag is more noticeable because the IP joint can hyperextend.11
Imaging
- Posteroanterior, oblique, and lateral radiograph views are recommended - The thumb can be a difficult bone to image. A Robert's view with hyperpronation of the extermity helps obtain an anteroposterior xray.
- Radiographs should be obtained before active motion testing to prevent potential displacement of an avulsed fracture fragment.
- MRI may also be useful for identifying mallet thumb injuries.
Treatment
- Due to the low incidence of mallet thumb, there is a lack of consensus on the optimal management strategy to address these injuries, and the role of surgery is not completely clear.11,14
- Treatment for both open and closed mallet thumb injuries varies from splinting of the IP joint alone to operative repair with or without temporary K-wire fixation of the IP joint.
- The prevailing opinion of most authors is to treat closed mallet thumb injuries nonsurgically with splinting—although there is still ongoing debate regarding this and the preferred type of splint is unclear—and to treat open injuries with primary tendon repair.12,14
- Conservative treatment is also indicated for fragments <30-40% of the joint surface or those with displacement of <2 mm.
- When surgery is indicated, the tendon is repaired after the IP joint is pinned in hyperextension. The K-wire is removed at 6 weeks postoperatively, and a splint is to be worn for the next 6 weeks, followed by nighttime splinting for another 4 weeks.14
- Cases in which the proximal severed EPL tendon retracts proximal to the IP joint may also necessitate surgery at the time of presentation, since a conservative approach to management could ultimately fail.12
- Other recommendations push for continuous extension splinting of the IP joint for 6 weeks unless there is volar subluxation of the distal phalanx.1
Complications
- Infection
- Posttraumatic osteoarthritis
Outcomes
- Data comparing operative and conservative approaches for mallet thumb injuries is also lacking, and although the literature demonstrates that most authors advocate for a conservative approach for closed injuries followed by splinting for 6-8 weeks, operative management in these cases is still advocated by some.12
- One study reported satisfactory results in 84% of mallet thumb patients treated with extension splinting, but noted that better outcomes occurred in those treated within 2 weeks of the injury, suggesting that early treatment may lead to superior outcomes. 8
- One trial suggested that the greater the gap between the severed tendons in mallet thumb injuries, the less likely conservative treatment will be at attaining a good outcome, especially if the severed end heals by approximating proximal to the IP joint.12
- Another study found that outcomes were similar between patients treated conservatively and surgically for mallet thumb injuries, with the only significant difference being immobilization time, which was 9.5 weeks in conservative patients compared to 4.9 weeks for surgical patients.15
IP joint fracture-dislocation
- Dislocations and fracture-dislocations of the IP joint are uncommon injuries owing to the joint’s inherent stability. These injuries usually occur after an axial load is applied to the thumb, causing the distal phalanx to be dorsally displaced and radially rotated.16-18
- A fracture-dislocation of the IP joint may also result in an avulsion fracture of the joint’s volar plate or the FPL tendon. A collateral ligament tear also can result from a volar plate avulsion.16
- The volar plate of the IP joint inserts on the volar base of the distal phalanx just proximal to the fan-like insertion of the FPL tendon. Sesamoid bones may be present in the volar plate just proximal to its thinner midline portion. Centrally, the thumb’s IP volar plate also becomes thinner and is loosely anchored to the periosteum of the proximal phalanx.17
Imaging
- Plain radiographs are usually sufficient, but an MRI may also be needed.
Treatment
- The treatment of IP joint fracture-dislocations is dependent on the size and degree of comminution of the intra-articular fragments.
- For small intra-articular fragments involving <25-40% of the articular surface, stable closed reduction is usually possible.
- For a single, large non-comminuted fragment, ORIF may be possible. If the large intra-articular fragment is comminuted, internal fixation may not be technically feasible. In this case, the treatment options are less clear.
- One option would involve temporary pinning in a reduced position followed by early motion.
- Other options include mobile or immobile external fixation devices. Primary arthrodesis could be considered as a last resort.17
- Surgical intervention may also be necessary if the patient fails closed reduction. Whether to perform temporary transarticular pinning should be determined by evaluating the stability by passive ROM and joint stability during the operation.16,18
- If the volar plate or FPL has entered the joint space, it may need to be surgically repaired or extricated.18
- Due to the anatomic similarity between the volar plates of the IP and PIP joints, a technique called Eaton volar plate arthroplasty may be appropriate for IP fracture-dislocations with volar plate avulsions.17
Complications
- Infection
- IP joint pain
- IP joint stiffness and flexion contractures
Outcomes
- Closed reduction of the IP joint has been found to be successful, especially with closed injuries. The most common reason for a failed reduction is avulsion of the volar plate with interposition into the IP joint.18
Related Anatomy
- The thumb distal phalanx consists of a distal bony tuft, a narrow diaphyseal shaft, a proximal metaphysis, and a base that articulates at the IP joint with the proximal phalanx. The base of the thumb distal phalanx has a dorsal and volar lip.
- Ligaments that attach to the thumb distal phalanx include the volar plate of the IP joint, the radial collateral ligament of the IP joint and the ulnar collateral ligament of the IP joint.
- Tendon attachments include the FPL tendon and the EPL tendon, which inserts at the dorsal tubercle of the distal phalanx base. Unlike the extensor digitorum communis, the EPL lacks any “true” lateral bands, and instead, fibers from the abductor pollicis brevis and adductor pollicis insert on the radial and ulnar sides of the tendon, respectively.12
- The thumb distal phalanx is further stabilized by fibrous septae in the pulp of the thumb and ulnar and radial lateral interosseous ligaments between the base and tuft of the thumb distal phalanx.
Incidence and Related injuries/conditions
- Metacarpal and phalangeal fractures account for nearly half of all hand injuries that present to the emergency room.19
- The most commonly fractured bone in the human hand is the distal phalanx.1,3
- The highest number of distal phalanx fractures occur in the long finger, followed by the thumb.4
- Fractures of the thumb are most common in the children and the elderly, with the thumb being the most commonly fractured tubular bone in elderly patients.20
- Thumb distal phalanx fractures most commonly occur secondary to sports in younger patients, secondary to labor in middle-aged patients, and secondary to falls and motor vehicle accidents in older individuals.10
- Mallet thumb injuries account for about 2-3% of all mallet finger injuries.13
- Subungual hematomas are a common related injury.