Fracture Nomenclature for Distal Radius Fractures
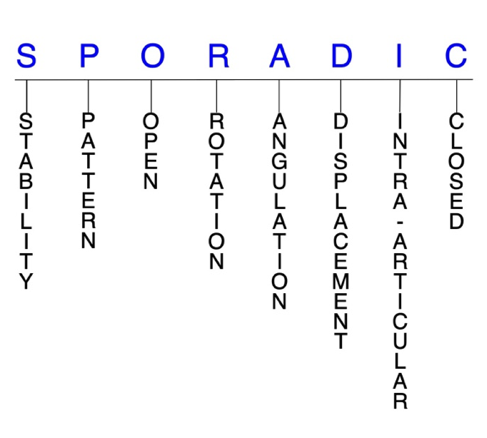
Hand Surgery Resource’s Diagnostic Guides describe fractures by the anatomical name of the fractured bone and then characterize the fracture by the Acronym:
In addition, anatomically named fractures are often also identified by specific eponyms or other special features.
For the Distal Radius, the historical and specifically named fractures include:
Colles’ Fracture
Smith Fracture
Barton Fracture
Reverse Barton Fracture
Distal ulna fracture
By selecting the name (diagnosis), you will be linked to the introduction section of this Diagnostic Guide dedicated to the selected fracture eponym.
Distal radius fractures account for 12-17% of all fractures, which makes them the most common upper extremity fracture. These injuries occur most frequently in two age groups: in children and adolescents due to high-energy trauma, and in older patients with osteopenia or osteoporosis after low-to-moderate energy injuries. Despite the high prevalence of distal radius fractures and the continued emergence of new treatment options and techniques, universal consensus on the optimal management strategy is lacking. Many distal radius fractures—especially closed, stable, nondisplaced injuries—can effectively be treated conservatively with closed reduction and immobilization. Surgery is often required for open and severely displaced fractures, and for those that fail conservative treatment.1-6,26-30
Definitions
- A distal radius fracture is a disruption of the mechanical integrity of the distal radius.
- A distal radius fracture produces a discontinuity in the distal radius contours that can be complete or incomplete.
- A distal radius fracture is caused by a direct force that exceeds the breaking point of the bone.
Hand Surgery Resource’s Fracture Description and Characterization Acronym
SPORADIC
S – Stability; P – Pattern; O – Open; R – Rotation; A – Angulation; D – Displacement; I – Intra-articular; C – Closed
S - Stability (stable or unstable)
- Universally accepted definitions of clinical fracture stability is not well defined in the literature.7-9
- Stable: fracture fragment pattern is generally nondisplaced or minimally displaced. It does not require reduction, and the fracture fragments’ alignment is maintained by with simple splinting or casting. However, most definitions define a stable fracture as one that will maintain anatomical alignment after a simple closed reduction and splinting. Some authors add that stable fractures remain aligned, even when adjacent joints are put to a partial range of motion (ROM).
- Unstable: will not remain anatomically or nearly anatomically aligned after a successful closed reduction and immobilization. Typically unstable distal radius fractures have significant deformity with comminution, displacement, angulation, and/or shortening.
- A distal radius fracture is further defined as unstable if it is unable to resist displacement after being anatomically reduced.10
P - Pattern
- Distal radial styloid
- Distal dorsal medial fragment
- Distal volar medial fragment
- Distal radial shaft
O - Open
- Open: a wound connects the external environment to the fracture site. The wound provides a pathway for bacteria to reach and infect the fracture site. As a result, there is always a risk for chronic osteomyelitis. Therefore, open fractures of the distal radius require antibiotics with surgical irrigation and wound debridement.7,11,12
R - Rotation
- Distal radius fracture deformity can be caused by proximal rotation of the fracture fragment in relation to the distal fracture fragment.
- Degree of malrotation of the fracture fragments can be used to describe the fracture deformity.
A - Angulation (fracture fragments in relationship to one another)
- Angulation is measured in degrees after identifying the direction of the apex of the angulation.
- Straight: no angulatory deformity
- Angulated: bent at the fracture site
- Extreme dorsal angulation may be associated with triangular fibrocartilage complex (TFCC) injuries.10
D - Displacement (Contour)
- Displaced: disrupted cortical contours
- Nondisplaced: ≥1 fracture line(s) defining one or several fracture fragments; however, the external cortical contours are not significantly disrupted
- In distal radius fractures, displacement can be either extra-articular or intra-articular. Extra-articular displacement can occur in any of the 3 planes. When displacement occurs in the sagittal plane, it typically leads to loss of the palmar tilt, while volar shear injuries tend to increase palmar tilt. In the coronal plane, displacement typically manifests as the loss of radial inclination and/or height.13
I - Intra-articular involvement
- Intra-articular fractures are those that enter a joint with ≥1 of their fracture lines.
- Distal radius fractures can have fragment involvement with the radiocarpal joint or distal radioulnar joint (DRUJ).
- If a fracture line enters a joint but does not displace the articular surface of the joint, then it is unlikely that this fracture will predispose to posttraumatic osteoarthritis. If the articular surface is separated or there is a step-off in the articular surface, then the congruity of the joint will be compromised and the risk of posttraumatic osteoarthritis increases significantly.
C - Closed
- Closed: no associated wounds; the external environment has no connection to the fracture site or any of the fracture fragments.4-6
Distal radius fractures: named fractures, fractures with eponyms and other special fractures
Colles’ fracture14-17
- Fractures of the distal radius were first accurately described by Abraham Colles as injuries that “take place at about an inch and a half above the carpal extremity of the radius” and “the carpus and the base of metacarpus appears to be thrown backward.” Although the eponym “Colles’ fracture” has been used to characterize this injury, more comprehensive, reliable, and prognostic classification systems have been introduced.
- A Colles’ fracture is an extra-articular, dorsally angulated fracture of the distal radius. The primary feature is dorsal displacement of the principal distal fracture fragment, and dorsal comminution, dorsal angulation, radial shortening, and associated ulnar styloid fractures are also common.10,18
- Colles’ fractures are extremely common, accounting for more than 90% of all distal radius fractures and are one of the most common types of fractures seen in Emergency Departments.19
- These fractures frequently occur in older adults with osteoporosis secondary to a fall onto an outstretched hand (FOOSH) injury, which forces the wrist into supination.
Imaging
- Radiology studies - X-ray
- Radiology studies - Computerized tomography (CT) scanning
- Electrophysiological testing - EMG/NCV
Treatment
Conservative
- A treatment algorithm should be used to determine whether conservative treatment is sufficient or if surgery is required. This algorithm should be based on whether the fracture is displaced or non-displaced, stable or unstable, and intra-articular or extra-articular.
- Conservative treatment for Colles’ fractures typically involves closed reduction and immediate immobilization with a sugar-tong splint, followed by casting. This approach is particularly applicable to stable, non-displaced fractures or fractures without significant intra-articular deformity.
Operative
- Extrafocal percutaneous pinning
- For extra-articular or simple intra-articular fractures.
- Arthroscopically assisted reductions
- Can be used to assess joint congruity and associated ligamentous injuries.
- Open reduction and internal fixation (ORIF) with fragment-specific fixation
- This technique uses low-profile implants to restore stability and articular congruity.
- ORIF with volar or dorsal plates for fixation
- Bone-graft substitutes
- Options include autologous or allogenic cancellous bone graft, demineralized bone matrix, calcium phosphate-based void fillers, autologous bone marrow fillers.
- External fixation (bridging, non-bridging) with closed reduction
Complications
- Injury-related
- Post-traumatic arthritis
- Nerve injury
- Stiffness
- Failure to maintain reduction
- Compartment syndrome
- Skin tearing during reduction
- Carpal tunnel syndrome
- Extensor pollicis longus (EPL) or flexor pollicis longus (FPL) rupture
- Splint/cast-related
- EPL rupture
- Carpal tunnel syndrome
- Loss of ROM
- Post-traumatic arthritis in radiocarpal joint or DRUJ
- Complex regional pain syndrome (CRPS)
- Surgery-related
- Nerve injury
- Soft-tissue injury
- Infection
- Late extensor or flexor tendon ruptures
Outcomes
- Worse outcomes are associated with axial shortening (>6 mm) during healing, comorbid injuries (eg, TFCC and scapholunate ligament tears), DRUJ instability, and work-related injuries.
- Fractures that heal with >20° of dorsal angulation, 10° of radial shortening, and/or 2 mm of articular incongruity also have a less favorable functional outcome.
Smith fracture
- Also known as a reverse Colles’ or volar Colles’ fracture, these are extra-articular distal radius fractures that involves volar displacement or angulation of a singular distal fragment.1,10,18,20
- Although Smith fractures are the second most common type of distal radius fractures, they are significantly less common than the Colles’ fracture.20
- Smith fractures most often occur either from a fall onto a flexed wrist—usually after falling backward and planting an outstretched hand behind the body—or due to a direct blow to the dorsal wrist. FOOSH injuries onto an outstretched palm may also be responsible in some cases.20
- A Smith type II fracture, also known as a Reverse Barton Fracture or volar type Barton fracture, is an intra-articular fracture with volar displacement of the distal radius. These fractures involve the volar lip and occur with the wrist in palmar flexion.3,20
Imaging20
- Radiology studies - X-ray
- Can help to differentiate between Colles’ and Smith fracture types.
- Anteroposterior (AP) and lateral are usually sufficient, but traction, oblique, and fossa lateral views may be required in some cases.
- Radiology studies - Computerized tomography (CT) scanning
- May be useful in the presence of extensive comminution or intra-articular fracture patterns.
Treatment1,20
Conservative
- For non-displaced, stable Smith fractures, the conservative treatment of choice is closed reduction followed by immobilization.
- The wrist should be reduced and splinted in extension, and a thermoplastic splint or brace can be used for acute fractures.
Operative
- Surgical indications in Smith fractures include dorsal or volar comminution, intra-articular involvement, residual instability after reduction, surface angulation greater than 20°, articular surface step-off of >2 mm, and radial shortening of >5 mm.
- ORIF
- Preferred surgical procedure for Smith fractures.
- Best choice for unstable or non-reducible fractures.
- Dorsal, volar, or fragment-specific
- Closed reduction with percutaneous pinning (CRPP)
- External fixation
Complications
- Malunion
- Garden spade deformity
- Pin track infection
- Pin loosening
- CRPS
- Carpal tunnel syndrome
- EPL rupture
Outcomes
- ORIF has been found to lead to significant improvements compared to conservative casting in cases of significant displacement or angulation, comminution, or in cases when the fracture remains unstable after reduction attempts.20
Barton fracture
- This is a dorsally or volarly displaced intra-articular fracture of the distal radius that also involves a subluxation or dislocation of the radiocarpal joint. Displacement occurs due to a triangular fragment of the dorsal or volar margin of the distal radius being sheared off and displaced from the carpus.1,10,18
- The Barton fracture is distinguished from Colles’ and Smith fractures because of the intra-articular radiocarpal joint involvement.10
- In pediatric and young adult patients, these injuries typically result from sporting activities and motor vehicle accidents. In older adults—particularly women—most Barton fractures result from falls in patients with osteoporosis.21
Imaging
- Radiology studies - X-ray
- Frontal and lateral views are most important. Oblique views may also help in reaching a diagnosis.21
- Radiology studies - Computerized tomography (CT) scanning
- May be utilized for better anatomic detail or when radiographs are unclear.21
- Magnetic resonance imaging - MRI without contrast
Treatment21
Conservative
- Non-displaced and stable Barton fractures should be treated with closed reduction and immobilization in a splint or cast; however, many of these fractures fail conservative treatment due to displacement. Therefore, most Barton fractures are treated surgically.
- An immobilization period of ≥6 weeks is typically required.
Operative
- The most common surgical intervention is closed reduction with external fixation, followed by percutaneous pinning.
Complications
- TFCC tears
- Carpal tunnel syndrome
- Forearm compartment syndrome
- CRPS
Outcome
- Although surgery is used more frequently for Barton fractures, research has shown that there are no significant differences in outcomes between conservative and operative treatment approaches.
- When surgery is performed, outcomes are generally better in young patients than in older adults.21
Distal ulna fracture22
- Isolated fractures of the distal ulna are relatively rare, but these injuries do frequently occur in conjunction with distal radius fractures.
- When distal ulnar and distal radius fractures occur concomitantly, the ulnar styloid is most commonly involved. Other injured structures may include the interosseous membrane (IOM), DRUJ, and TFCC. Due to the complex interaction between these bones and supporting structures, diagnosing and treating combined distal radius and ulna fractures is often challenging.
Imaging
- Radiology studies - X-ray
- Radiology studies - Computerized tomography (CT) scanning
- May be needed to accurately define fracture fragments.
- Magnetic resonance imaging - MRI without contrast
- May be considered if the physician suspects a TFCC injury or ligamentous disruption of the DRUJ.
Treatment
Conservative
- Conservative treatment is usually recommended for most ulnar styloid fractures, as well as for older adults with distal ulna metaphyseal fractures combined with a distal radius fracture and a stable DRUJ.
- Immobilization with casting may also be used for isolated distal ulna shaft and metaphyseal fractures with <50% displacement.
Operative
- In general, surgery is primarily recommended for the ulnar styloid if there is DRUJ instability or the fracture is comminuted and extends into the DRUJ.
- Ulnar styloid ORIF
- Fixation methods/hardware
- Kirschner wires
- Tension banding
- Intraosseous wiring
- Plate-screw constructs
- Lag screw fixation
Complications
- Nonunion
- Neurapraxia
- DRUJ arthrosis
- Ulnar impaction
Outcomes
- Research suggests that functional outcomes for distal radius fractures are not negatively impacted by the presence of ulnar styloid fractures or failure to repair it.
- No method of fixation or immobilization has been found to be superior for isolated diaphyseal fractures.
Related Anatomy1,23
- Distal radius, Radiocarpal joint, Lister’s tubercle and Distal radioulnar joint (DRUJ)
- The radius consists of a radial head and radial neck at its proximal end. The shaft of the radius then extends from the neck and has a rectangular epiphysis on its distal end. The articular—or lateral—surface of the distal radius is biconcave and triangular, and the apex of this triangle is directed toward the styloid process. On the medial surface, there is a concavity called the ulnar notch that articulates with the head of ulna, forming the DRUJ. The distal surface of the radius has two facets for articulation with the scaphoid and lunate carpal bones. There is also an articulation between the distal radius and the triquetral bone facilitated by a biconcave articular disc. Collectively, these three articulations form the radiocarpal joint.
- Ligaments associated with the distal radius include the dorsal radiocarpal ligament, which spans the ulnar aspect of the dorsal rim of the distal radius from the ulnar margin of the Lister tubercle to the sigmoid notch; the radioscaphocapitate ligament, which originates from the radial styloid and spans to the volar rim of the distal radius at the scaphoid fossa; the long radiolunate ligament, which originates from the volar rim of the scaphoid fossa; and the short radiolunate ligament, which originates from the volar rim of the lunate fossa.
- Tendons associated with the distal radius include those associated with the extensor carpi radialis brevis (ECRB), extensor carpi radialis longus (ECRL), and EPL muscles. The dorsal tubercle protrudes on the posterior aspect of the distal head of the radius and is seated between the grooves for the tendons of the ECRB and ECRL as well as the tendon of the EPL.
- The radius and ulna are connected by a sheet of thick fibrous tissue called the IOM.
Incidence
- Distal radius fractures are one of the most prevalent orthopaedic injuries and represent the most common of all upper extremity fractures, accounting for 12-17% of all fractures.2,3,13
- Distal radius fractures follow bimodal age distribution during youth and adolescence (when high-energy trauma is usually responsible) and in older age (when low-to-moderate energy injuries usually lead to fractures in patients with osteopenia or osteoporosis).4,5
- The risk for distal radius fractures is about 4-5 times greater in women than in men. Postmenopausal women have the greatest lifetime risk for these injuries, and approximately 10% of women aged ≥65 years will sustain a distal radius fracture at some point in the remainder of their lifetime.2,5
- Osteoporosis accounts for ~250,000 wrist fractures annually
