Fracture Nomenclature for Thumb Proximal Phalanx Fracture
Hand Surgery Resource’s Diagnostic Guides describe fractures by the anatomical name of the fractured bone and then characterize the fracture by the Acronym:
In addition, anatomically named fractures are often also identified by specific eponyms or other special features.
For the Thumb Proximal Phalanx Fracture, the historical and specifically named fractures include:
Ulnar collateral ligament avulsion fracture/bony skier’s thumb/Gamekeeper's fracture
RCL avulsion fracture
MP joint fracture-dislocation with volar plate avulsion fracture
MP joint sesamoid bone fracture
By selecting the name (diagnosis), you will be linked to the introduction section of this Diagnostic Guide dedicated to the selected fracture eponym.
Fractures of the proximal phalanx of the thumb are less common than those of the thumb distal phalanx and metacarpal. These injuries are particularly prevalent in sports and are often the result of direct blunt trauma or from a fall on an outstretched hand (FOOSH).1
Definitions
- A thumb proximal phalanx fracture is a disruption of the mechanical integrity of the proximal phalanx.
- A thumb proximal phalanx fracture produces a discontinuity in the proximal phalanx contours that can be complete or incomplete.
- A thumb proximal phalanx fracture is caused by a direct force that exceeds the breaking point of the bone.
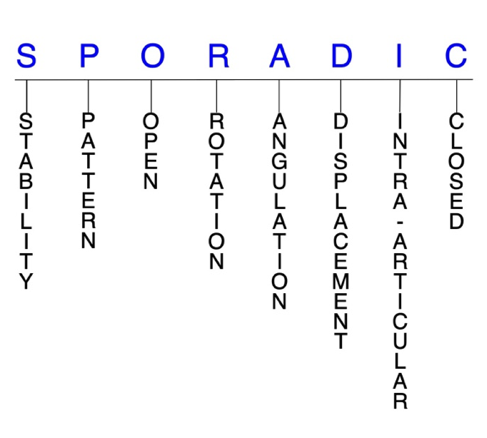
Hand Surgery Resource’s Fracture Description and Characterization Acronym
SPORADIC
S – Stability; P – Pattern; O – Open; R – Rotation; A – Angulation; D – Displacement; I – Intra-articular; C – Closed
S - Stability (stable or unstable)
- Universally accepted definitions of clinical fracture stability is not well defined in the hand surgery literature.2-4
- Stable: fracture fragment pattern is generally nondisplaced or minimally displaced. It does not require reduction, and the fracture fragments’ alignment is maintained with simple splinting. However, most definitions define a stable fracture as one that will maintain anatomical alignment after a simple closed reduction and splinting. Some authors add that stable fractures remain aligned, even when adjacent joints are put to a partial range of motion (ROM).
- Unstable: fracture will not remain anatomically or nearly anatomically aligned after a successful closed reduction and simple splinting. Typically unstable thumb proximal phalanx fractures have significant deformity with comminution, displacement, angulation, and/or shortening.
P - Pattern
- Thumb proximal phalanx head: oblique, transverse, or comminuted; can involve the interphalangeal (IP) joint; these are intra-articular fractures that affect one or both condyles of the thumb proximal phalanx head, with or without displacement; displaced fractures can affect joint congruity.
- Thumb proximal phalanx shaft: transverse, oblique, or comminuted with or without shortening.
- Thumb proximal phalanx base: can involve the metacarpophalangeal (MP) joint; fractures at the thumb proximal phalanx base are frequently concomitant with avulsions fractures of ligaments associated with the MP joint.5-7
O - Open
- Open: a wound connects the external environment to the fracture site. The wound provides a pathway for bacteria to reach and infect the fracture site. As a result, there is always a risk in developing osteomyelitis. Therefore, open fractures of the thumb proximal phalanx require antibiotics with surgical irrigation and wound debridement.2,8,9
R - Rotation
- Thumb proximal phalanx fracture deformity can be caused by proximal rotation of the fracture fragment in relation to the distal fracture fragment.
- Degree of malrotation of the fracture fragments can be used to describe the fracture deformity; this is not a common type of fracture deformity in the thumb proximal phalanx.
A - Angulation (fracture fragments in relationship to one another)
- Angulation is measured in degrees after identifying the direction of the apex of the angulation.
- Straight: no angulatory deformity
- Angulated: bent at the fracture site
- Example: unlike the finger phalanges, some angular displacement or malunion is acceptable in thumb proximal phalanx fractures due to the compensatory motion of the MP joint; therefore, angular deformities of up to 20° in the frontal plane and 30° in the lateral plane may be functionally well tolerated in these fractures.5
D - Displacement (Contour)
- Displaced: disrupted cortical contours (eg, thumb proximal phalanx shaft fractures can be displaced or translated partially or completely)
- Nondisplaced: fracture line defining one or several fracture fragments; however, the external cortical contours are not significantly disrupted
I - Intra-articular involvement
- Fractures that enter a joint with one or more of their fracture lines. Intra-articular fractures of the thumb proximal phalanx require special attention due to the digit’s indispensible role in hand function.9
- Thumb proximal phalanx fractures can have fragment involvement with the IP or MP joints.
- If a fracture line enters a joint but does not displace the articular surface of the joint, then it is unlikely that this fracture will predispose to posttraumatic osteoarthritis. If the articular surface is separated or there is a step-off in the articular surface then the congruity of the joint will be compromised and the risk of posttraumatic osteoarthritis increases significantly.
C - Closed
- Closed: no associated wounds; the external environment has no connection to the fracture site or any of the fracture fragments.2-4
Thumb distal phalanx fractures: named fractures, fractures with eponyms and other special fractures
Ulnar collateral ligament avulsion fracture/bony skier’s thumb/Gamekeeper's fracture
- Injuries to the ulnar collateral ligament (UCL) occur due to hyperabduction and forceful radial deviation of the thumb MP joint, and they are particularly common in contact sports and skiing.8
- An acute injury to the UCL is commonly called “skier’s thumb,” since it often results from a ski pole keeping the thumb in an abducted position, which increases its risk for excessive radial deviation. Skier’s thumb can also occur in ball or stick sports or from a FOOSH.
- The estimated annual incidence of skier’s thumb in the US is ~200,000.10
- The majority of skier’s thumb injuries result in a distal avulsion fracture of the UCL, and about 50% of all UCL injuries will have an associated fracture at the base of the thumb proximal phalanx. The term “bony skier’s thumb” may be used to describe a UCL avulsion fracture.6
- A chronic UCL injury is commonly referred to as “gamekeeper’s thumb,” as the injury was first identified in Scottish gamekeepers who experienced chronic ligament insufficiency consequential of their method for breaking the necks of rabbits between the thumb and index finger.
- This chronic injury can also result in a UCL avulsion fracture, and is approached in a similar manner to its conservative counterpart.6
- UCL injuries occur significantly more frequently than radial collateral ligament (RCL) injuries.5
- Displacement of the UCL proximal and superficial to the leading edge of the adductor pollicis aponeurosis is termed a Stener lesion. In these injuries, the aponeurosis of the adductor pollicis is interposed between the UCL and its insertion on the proximal phalanx, which prohibits healing.
- Accurate diagnosis of Stener lesions is often a diagnostic dilemma, since they often occur in the absence of a substantial bony fragment.5
- Some investigators have described a palpable mass proximal to the MP joint as a sign of a Stener lesion and occasionally an associated avulsion fracture with the fragment proximal to the location of the adductor hood will indicate a “bony Stener” lesion.6
Imaging
- Plain anteroposterior and lateral X-ray views of the thumb are recommended.
- Arthrogram
- Ultrasound
- MRI
Treatment
- Treatment for thumb UCL avulsion fractures is controversial, since many of these injuries are capable of primary healing if minimally displaced, and the available literature supports both conservative and surgical management strategies.5
- In general, the research suggests that undisplaced or minimally displaced avulsion fractures with no joint instability should be managed conservatively.11
- Conservative treatment should involve a thumb spica cast that includes the wrist until initial inflammation has resolved, followed by a thermoplastic splint that allows movement at the IP joint.
- The position of the splint involves holding the MP joint in slight flexion with gentle stressing in ulnar deviation. During immobilization, the patient should undergo supervised hand therapy.12
- Gentle flexion/extension exercises can begin after 4 weeks with the splint being worn between sessions, and the splint should remain on at all times apart from during therapy sessions for 6 weeks. Progressive strengthening exercises may begin after 8 weeks, and unrestricted activity is allowed after 12 weeks.12
- On the other hand, ORIF should be performed if: 1) 20% or greater of the joint surface is involved, 2) there is considerable fracture displacement, or 3) there is substantial instability with UCL testing. The goal of surgery is stable fixation that permits early motion.5,11
- The presence of a Stener lesion is another indication for surgical intervention.5
- If the fracture fragment is displaced more than 2 mm and the MP joint is unstable to stress, stability needs to be restored surgically.
- If the fracture fragment is small or breaks during internal fixation, it can be removed and the ligament reinserted with a pull-out suture or suture anchor.
- Larger fragments can be fixed with either K-wires or a small screw. The repair is protected with a transarticular smooth K-wire and thumb spica cast immobilization for 4-6 weeks.1
- Tension band wiring is a useful technique for fragments not large enough to support a screw, while suture anchors are recommended for smaller and comminuted fractures.11
- If there is any doubt about joint stability, stress testing should be performed under a median and radial nerve wrist block with the thumb at 30° MP flexion. If the joint opens 35° or more with radial deviation stress, then surgery is indicated.11
- For some surgeons, the presence of a displaced avulsion fracture is an indication for surgical intervention even if it is not displaced enough to be superficial to the adductor aponeurosis.13
Complications
- MP joint instability
- Nonunion
- Impaired grip/pinch strength
- Posttraumatic osteoarthritis
Outcomes
- Several studies have reported complete stability and no pain in a 63-100% of patients after being treated conservatively for nondisplaced UCL avulsion fractures.13
- Good outcomes were found in one study of 30 patients with UCL avulsion fractures treating conservatively, with 19 patients pain-free, 10 with mild pain, and 1 with moderate pain. Impairments in stability and grip/pinch strength were also rare. The authors of this study therefore recommend conservative treatment for most acute UCL avulsion fractures.14
- Conversely, another study found identified potential problems of conservatively treating small, minimally displaced UCL avulsion fractures, with 9 patients initially treated with cast immobilization experiencing persistent pain and diminished pinch and grip strength after at least 6 weeks in the cast. Late UCL reconstruction was subsequently performed in all patients with K-wire fixation and pull-through sutures, and subsequent outcomes were good.15
- Another study found that a hook plate construct was biomechanically superior and provided superior fixation of UCL avulsion fractures compared to the suture anchor construct. Hook plating may therefore allow an earlier return to forceful pinch activities and also provide a greater resistance to catastrophic failure in the early postoperative period for non-compliant or highly active patients.7
RCL avulsion fracture
- The RCL plays a significant role in stabilizing the MP joint, but injuries and avulsion fractures of this ligament are far less common than those of the UCL. RCL avulsion fractures typically occur due to forced adduction or torsion of the flexed thumb, which can occur in sports like handball or soccer, or from a FOOSH. Evaluation, diagnosis, and management is similar to that for UCL injuries, but there are several key differences between the two:16
- In contrast with the adductor aponeurosis, the abductor aponeurosis on the radial side of the thumb is broad and does not become interposed between the ligament and avulsed insertion site. As a result, equivalents of Stener lesions in RCL avulsion fractures are extremely rare.17
- Similarly, the location of RCL injuries is more variable. Most frequently, the ligament is avulsed from its proximal origin on the metacarpal as opposed to its distal insertion on the proximal phalanx.
- Midsubstance tears of the RCL are more common than midsubstance tears of the UCL.17
- Joint subluxation is more common with RCL injuries owing to the adductor pollicis insertion on the proximal phalanx and ulnar sesamoid. These insertions lie volar to the MP joint axis of rotation, causing a volar and ulnar-deforming force on the proximal phalanx.6
Imaging
- Anteroposterior and lateral X-ray views are recommended.
- Arthrogram
- Ultrasound
- MRI
Treatment
- Both conservative and surgical intervention strategies have been utilized for RCL avulsion fractures, with both options being well supported in the literature if the fracture is minimally displaced.6
- Non-displaced, non-rotated avulsed fragments are usually treated non-surgically, while displaced or rotated fragments should undergo surgical treatment. However, consistent recommendations and algorithms for optimal management of these injuries are yet to be delineated.6
- Though rare, Stener-like lesions on the radial side are also indications for surgery.6
- To date, two methods for surgical repair are mainly conducted: reduction and fixation or excision of the bony fragment, depending on fragment characteristics.16
- Rigid fixation of the fragment can be performed with a tension band construct or a 1.5-mm interfragmentary screw. If there are multiple small fragments, excision of those fragments with reattachment of the insertion of the RCL can be performed.6
- Osteosynthesis with ORIF is indicated except when a fragment is not displaced and the size of a fragment is very small.18
Complications
- MP joint instability
- Impaired pinch/grip strength
- Posttraumatic osteoarthritis
Outcomes
- Osteosynthesis was found to lead to bony union and good functional results with no complications and high satisfaction rates in patients with both UCL and RCL avulsion fractures.18
- In one study on patients with RCL avulsion fractures, 9 were treated surgically and 21 were treated non-surgically following a devised treatment algorithm. Outcomes were similar between groups, with 90.5% of patients in both groups being graded as “excellent” after treatment. There were also no significant between-group differences in post-treatment ROM.16
MP joint fracture-dislocation with volar plate avulsion fracture
- Traumatic dislocation of the thumb MP joint is considered a rare injury, but this may be due to it being underreported in the literature. The usual mechanism of injury is a FOOSH that causes forcible hyperextension of the joint. Dorsal dislocations are more frequent than volar dislocations, and MP joint dislocations are less common than IP dislocations.
- Concomitant fractures of the base of the proximal phalanx and metacarpal head occur in about 50% of MP joint dislocations.
- A fracture-dislocation of the thumb MP can also lead to avulsion of the volar plate, which is avulsed from its attachment on the metacarpal neck during MP hyperextension.
- In a simple dislocation, the volar plate is not interposed within the MP joint, and the base of the proximal phalanx remains in contact with the articular surface of the metacarpal head.
- In a complex dislocation, the volar plate becomes inserted into the MP joint, and open reduction is usually needed.19
Imaging
- Anteroposterior, lateral, and oblique X-ray views are recommended.
Treatment
- Unlike UCL avulsion fractures, a volar plate avulsion is considered a stable injury, and these injuries should be treated conservatively whenever feasible.11
- Some simple fracture-dislocations can be reduced non-surgically with initial MP hyperextension followed by dorsal pressure on the proximal phalanx in conjunction with wrist flexion.19
- Complex MP fracture-dislocations typically require open surgical reduction.20
- Simple distraction as a reduction maneuver is usually unsuccessful and can inadvertently convert a reducible dislocation into an irreducible one, as traction on the MP joint can draw the entire volar plate dorsally so that it can be completely folded between the base of the thumb proximal phalanx and metacarpal head.19
- When the volar plate becomes entrapped within the MP joint in an avulsion fracture, a closed reduction maneuver cannot be completed.19
- Because the anatomy of the thumb is different from that of the other fingers, dislocations requiring surgical intervention frequently involve interposition of the volar plate, sesamoid bones, or flexor pollicis longus tendon.19
Complications
- Posttraumatic osteoarthritis
- Osteonecrosis
- MP joint arthofibrosis/stiffness
- Decreased ROM
Outcomes
- Dorsal dislocations of the thumb MP joint are treated by the same reduction maneuver as the other fingers, but treatment has been found to be more likely to be successful in the thumb.19
MP joint sesamoid bone fracture
- Two sesamoid bones are present at the MP joint of thumb in more than 99% of people, and their function is probably to protect and stabilize the flexor tendons and intrinsic muscles of the hand. Fractures of either of these bones are very uncommon and can be easily missed in a diagnosis.21
- The most common mechanism of injury for MP joint sesamoid bone fractures is a violent hyperextension or hyperabduction of the thumb after a FOOSH, which may be related to sports. They may also result from direct trauma.21,22
- The volar plate can also be torn with or without an avulsion fracture in these injuries.22
- Sesamoid bone fractures are generally classified into two types:
- Type 1: the volar plate and MP joint remain intact.
- Type 2: rupture of the volar plate with associated thumb hyperextension.21
Imaging
- Since sesamoid fractures may not be evident on routine anteroposterior and lateral views, oblique views should be obtained when this type of fracture is suspected.
- Ultrasound may be particularly useful to detect sesamoid fractures that are clinically or radiographically overlooked.
- CT scan may also be necessary.
Treatment
- It is important to diagnose and treat sesamoid bone fractures as early as possible, since these injuries can be easily missed.21
- Type 1 sesamoid bone fractures can be treated conservatively with immobilization of the thumb and the MP joint in 30° of flexion for 2-4 weeks. Taping may also be sufficient. If pain and discomfort persist after adequate conservative treatment, excision of the bone may be needed.21,23
- Type 2 fractures may require surgical reduction of the MP joint and sesamoid fracture and repair of the volar plate if the fracture is complicated and instability of the MP joint is clinically demonstrated.21,23
- Other recommendations call for conservative treatment of closed sesamoid fractures and surgical treatment for open fractures, in which the fracture fragments are approximated to reinforce the volar plate repair to prevent a hyperextension deformity of the MP joint.23
Complications
Outcomes
- The prognosis for a sesamoid bone fracture is good when it is properly diagnosed at an early stage, but poor functional outcomes are common when the injury is missed.
- Taping has been associated with positive overall outcomes and no complications in one study.23
Related Anatomy
- The thumb proximal phalanx consists of a distal phalangeal head that articulates at the IP joint with the distal phalanx, a narrow diaphyseal shaft, a proximal metaphysis, and a base that articulates at the MP joint with the metacarpal. The base of the thumb proximal phalanx also has a dorsal and volar lip.
- The ligaments associated with the thumb proximal phalanx at the IP and MP joints are the joint capsule, the UCL and RCL (proper and accessory collaterals), and the volar plates.
- Tendon attachments include the abductor pollicis brevis, flexor pollicis brevis, and opponens pollicis.
Incidence and Related injuries/conditions
- Metacarpal and phalangeal fractures account for nearly half of all hand injuries that present to the emergency room.24
- Phalangeal fractures account for 23% of all below-elbow fractures.25
- Fractures of the thumb are most common in children and the elderly, with the thumb being the most commonly fractured tubular bone in elderly patients.26
- Thumb proximal phalanx fractures most commonly occur secondary to sports in younger patients, secondary to labor in middle-aged patients, and secondary to falls and motor vehicle accidents in older individuals.9
- The estimated annual incidence of skier’s thumb in the U.S. is ~200,000.10