Fracture Nomenclature for Pediatric Radial Head fractures
Hand Surgery Resource’s Diagnostic Guides describe fractures by the anatomical name of the fractured bone and then characterize the fracture by the Acronym:
In addition, anatomically named fractures are often also identified by specific eponyms or other special features.
For the Pediatric Radial Head Fractures, the historical and specifically named fractures include:
Jeffery type 2 fracture
By selecting the name (diagnosis), you will be linked to the introduction section of this Diagnostic Guide dedicated to the selected fracture eponym.
The elbow is common site for injury in children and adolescents, but only about 4–16% of elbow fractures involve the radial head or neck. Radial head and neck fractures most commonly occur in children aged 9–10 years, and the typical mechanism of injury is a fall on an outstretched hand that produces a valgus compressive force across the elbow. Isolated fractures of the radial head or neck are extremely rare, while concomitant elbow dislocations and medial epicondyle fractures are more likely. Extraarticular fractures occur more frequently than intraarticular fractures because the radial head is still primarily cartilaginous in younger ages. Most pediatric radial head and neck fractures can be treated successfully with closed reduction and/or immobilization only, while severely displaced and/or angulated fractures often require surgery.1-6
Definitions
- A pediatric radial head fracture is a disruption of the mechanical integrity of the pediatric radial head.
- A pediatric radial head fracture produces a discontinuity in the distal humeral contours that can be complete or incomplete.
- A pediatric radial head fracture is caused by a direct force that exceeds the breaking point of the bone.
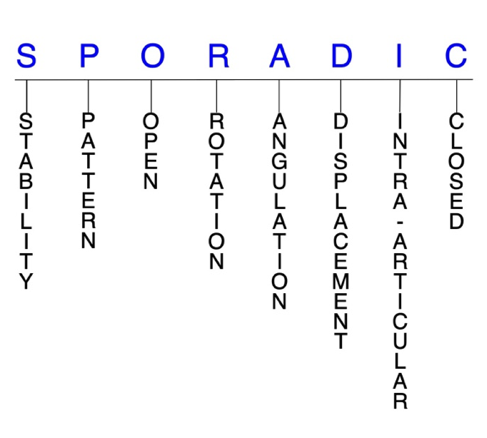
Hand Surgery Resource’s Fracture Description and Characterization Acronym
SPORADIC
S – Stability; P – Pattern; O – Open; R – Rotation; A – Angulation; D – Displacement; I – Intra-articular; C – Closed
S - Stability (stable or unstable)
- Universally accepted definitions of clinical fracture stability are not well defined in the literature.7-9
- Stable: fracture fragment pattern is generally nondisplaced or minimally displaced. It does not require reduction, and the fracture fragments’ alignment is maintained by with simple splinting or casting. However, most definitions define a stable fracture as one that will maintain anatomical alignment after a simple closed reduction and splinting. Some authors add that stable fractures remain aligned, even when adjacent joints are put to a partial range of motion (ROM).
- Unstable: will not remain anatomically or nearly anatomically aligned after a successful closed reduction and immobilization. Typical unstable pediatric radial head fractures have significant deformity with comminution, displacement, angulation, and/or shortening.
P - Pattern2
- Several classification systems may be used in the diagnosis of pediatric radial head and neck fractures, which classify fractures based on displacement, anatomic location, or configuration. Among the most frequently used are the Judet classification and the Wilkins classification systems, with most authors preferring the Judet system.
- Judet classification system for radial neck fractures
- Type I: nondisplaced
- Type II: angulation <30°, translation <50%
- Type III: angulation 30–60°, translation 50–100%
- Type IV: angulation >60°, translation >100%
- Wilkins classification system for radial neck fractures
- Grade A: Salter-Harris I or II physeal fracture
- Grade B: Salter-Harris III or IV intra-articular fracture
- Grade C: metaphyseal fracture
O - Open
- Open: a wound connects the external environment to the fracture site. The wound provides a pathway for bacteria to reach and infect the fracture site. As a result, there is always a risk for chronic osteomyelitis. Therefore, open fractures of the pediatric radial head or neck require antibiotics with surgical irrigation and wound debridement.7,10,11
R - Rotation
- Pediatric radial head fracture deformity can be caused by proximal rotation of the fracture fragment in relation to the distal fracture fragment.
- Degree of malrotation of the fracture fragments can be used to describe the fracture deformity.
A - Angulation (fracture fragments in relationship to one another)
- Angulation is measured in degrees after identifying the direction of the apex of the angulation.
- Straight: no angulatory deformity
- Angulated: bent at the fracture site
D - Displacement (Contour)
- Displaced: disrupted cortical contours
- Nondisplaced: ≥1 fracture lines defining one or several fracture fragments; however, the external cortical contours are not significantly disrupted
I - Intra-articular involvement
- Intra-articular fractures are those that enter a joint with ≥1 of their fracture lines.
- Pediatric radial head and neck fractures can have fragment involvement at the proximal radioulnar joint or radiocapitellar joint.
- If a fracture line enters a joint but does not displace the articular surface of the joint, then it is unlikely that this fracture will predispose to posttraumatic osteoarthritis. If the articular surface is separated or there is a step-off in the articular surface, then the congruity of the joint will be compromised, and the risk of post-traumatic osteoarthritis increases significantly.
- Intraarticular fractures of the radial head are relatively rare in children because the radial head is primarily cartilaginous until the proximal epiphysis begins to close around 14–15 years in boys and 12–14 years in girls.1
C - Closed
- Closed: no associated wounds; the external environment has no connection to the fracture site or any of the fracture fragments.4-6
Pediatric radial head fractures: named fractures, fractures with eponyms and other special fractures
Jeffery type 2 fracture
- Also known as the Jeffery type 2 lesion, this injury involves a radial neck fracture with a posterior subluxation or dislocation of the radiocapitellar joint.12,13
- Jeffery type 2 fractures result from the impact of the capitellum on the anterior lip of the radial head, creating a 90° backward tilt of the radial head.12,13
- This type of injury is uncommon but can lead to dangerous consequences if not recognized or properly treated.14
Imaging
- Radiology studies - X-ray
- Anteroposterior (AP) and lateral radiographs of the elbow are recommended.14
Treatment13,14
- Closed or percutaneous reduction
- May be considered in some cases.
- Open reduction and internal fixation (ORIF)
- Typically recommended due to the risks associated with percutaneous and closed reductions.
Complications
- Avascular necrosis
- Premature physeal closure
- Radial head overgrowth
- Radioulnar synostosis
Outcomes
- ORIF has been associated with early recovery and good clinical outcomes in two case series.12,13
- Closed reduction frequently is often unsuccessful and may lead to an upside down displacement of the radial head12; however, one case report found that a 10-year-old patient treated conservatively with closed reduction experienced excellent radiological and clinical results.14
Related Anatomy3,4,15-19
- The elbow is a hinge-type synovial joint comprised of the radius, ulna, and humerus, and formed by three articulations: the ulnohumeral joint, radiocapitellar joint, and proximal radioulnar joint (PRUJ).
- The radiocapitellar joint is the articulation of the radial head with the capitellum of the humerus. It is essential to elbow longitudinal and valgus stability and has an integral relationship with the LCL.
- The radius consists of a rectangular epiphysis at its distal end, a long shaft, and a radial neck and head at its proximal end. The radial head is important because it influences all three elbow articulations. The stability of the radiocapitellar joint is based on the opposite congruity of the convex capitellum with the concave radial head. Articular cartilage covers this concave surface and at least an arc of ~280° around the rim of the radial head.
- The PRUJ is formed by the articulation of the radial head with the lesser sigmoid notch of the proximal ulna and is stabilized by the annular ligament.
- The key ligaments of the elbow include the LCL (which extends from the lateral epicondyle and blends with the annular ligament of the radius), the MCL (which originates from the medial epicondyle and attaches to the coronoid process and olecranon of the ulna), and the annular ligament (which encircles the radial head and stabilizes the PRUJ and radiocapitellar joint).
- The key tendons of the elbow include the tendons associated with the biceps, triceps, extensor carpi radialis brevis (ECRB), and extensor carpi radialis longus (ECRL) muscles.
- The radius and ulna are also connected by a sheet of thick fibrous tissue called the IOM.
- There are six ossification centers around the elbow joint, which ossify at different ages in a child’s development. These centers and the approximate age of ossification are as follows:
- Capitellum: 1 year
- Radial head: 3 years
- Internal or medial epicondyle: 5 years
- Trochlea: 7 years
- Olecranon: 9 years
- External or lateral epicondyle: 11 years
- The radial head fuses with the radial shaft between ages 16–18.
- The proximal radius growth plate is responsible for only 20–30% of the radius’ growth.
Incidence
- Radial head and neck fractures account for 4–16% of all elbow injuries and <1% of all fractures in the pediatric population.1
- The average age for pediatric radial head and neck fractures is 9–10 years.3,5
- Most of these fractures involve the extraarticular and/or metaphyseal regions of the proximal radius, usually occurring as Salter-Harris type II fractures that transect the physis and extend into the metaphysis. Intraarticular fractures are uncommon at younger ages. 1,20
