Fracture Nomenclature for Finger Distal Phalanx Fractures Pediatric
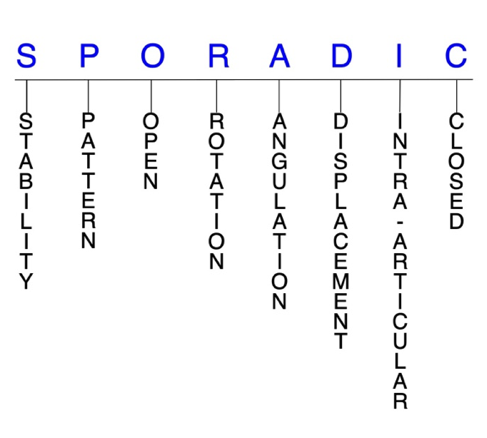
Hand Surgery Resource’s Diagnostic Guides describe fractures by the anatomical name of the fractured bone and then characterize the fracture by the Acronym:
In addition, anatomically named fractures are often also identified by specific eponyms or other special features.
For the Finger Distal Phalanx Pediatric, the historical and specifically named fractures include:
Seymour fracture
Mallet finger fracture
FDP tendon avulsion fracture
By selecting the name (diagnosis), you will be linked to the introduction section of this Diagnostic Guide dedicated to the selected fracture eponym.
Fractures of the hand are the most common type of fracture sustained by children, and the majority of these occur in the phalanges, with the proximal phalanx being most frequently affected, followed by the distal phalanx. The cause of these injuries varies and is largely dependent on the age of the child, with crush injuries being common in toddlers and sports participation often responsible in older children and adolescents. Although pediatric distal phalanx fractures share several similarities with their counterparts in the adult population, the presence of physes and other developmental changes necessitates special consideration. Thus, the diagnosis and management of certain pediatric distal phalanx fractures can differ substantially from that for adults.1-6
Definitions
- A pediatric distal phalanx fracture is a disruption of the mechanical integrity of the distal phalanx.
- A pediatric distal phalanx fracture produces a discontinuity in the distal phalanx contours that can be complete or incomplete.
- A pediatric distal phalanx fracture is caused by a direct force that exceeds the breaking point of the bone.
Hand Surgery Resource’s Fracture Description and Characterization Acronym
SPORADIC
S – Stability; P – Pattern; O – Open; R – Rotation; A – Angulation; D – Displacement; I – Intra-articular; C – Closed
S - Stability (stable or unstable)
- Universally accepted definitions of clinical fracture stability is not well defined in the hand surgery literature.7-9
- Stable: fracture fragment pattern is generally nondisplaced or minimally displaced. It does not require reduction, and the fracture fragments’ alignment is maintained with simple splinting. However, most definitions define a stable fracture as one that will maintain anatomical alignment after a simple closed reduction and splinting. Some authors add that stable fractures remain aligned, even when adjacent joints are put to a partial range of motion (ROM).
- Unstable: will not remain anatomically or nearly anatomically aligned after a successful closed reduction and simple splinting. Typically unstable pediatric distal phalanx fractures have significant deformity with comminution, displacement, angulation, and/or shortening.
- In the pediatric population, even the displaced fractures can be easily reduced closed and often are stable.3
P - Pattern
- Distal phalanx tuft: The oblique, transverse, and comminuted fractures are the most common distal phalanx fracture patterns. Tuft fractures usually result from crush injuries, and they are often comminuted but stable and minimally displaced. Tuft fractures are nearly always associated with an injury to the nail matrix, digit pulp, or both.5,10,11
- Distal phalanx shaft: transverse, oblique, or comminuted with or without shortening.
- Distal phalanx base: can involve the distal interphalangeal (DIP) joint; may be intra- or extra-articular; intra-articular fractures are due to extensor digitorum tendon avulsion injury or flexor digitorum profundus (FDP) tendon avulsion injury. These fractures usually involve the dorsal or volar lip of the distal phalanx base.11
O - Open
- Open: a wound connects the external environment to the fracture site. The wound provides a pathway for bacteria to reach and infect the fracture site. As a result, there is always a risk for chronic osteomyelitis. Therefore, open fractures of the pediatric distal phalanx require antibiotics with surgical irrigation and wound debridement.7,12,13
- Since Seymour fractures involve an associated nail bed laceration, most are technically considered open fractures.1
R - Rotation
- Pediatric distal phalanx fracture deformity can be caused by proximal rotation of the fracture fragment in relation to the distal fracture fragment.
- Degree of malrotation of the fracture fragments can be used to describe the fracture deformity. This is not a common type of fracture deformity in the pediatric distal phalanx.
- Oblique fractures of the small finger are often malrotated, although physeal, transverse, intra-articular, and minor fractures by radiographic appearance can also be malrotated and lead to a rotated malunion.4
A - Angulation (fracture fragments in relationship to one another)
- Angulation is measured in degrees after identifying the direction of the apex of the angulation.
- Straight: no angulatory deformity
- Angulated: bent at the fracture site
- Example: Seymour fractures typically result from a volar force and a dorsal apex angulation of the diaphysis compared with the epiphysis.1
D - Displacement (Contour)
- Displaced: disrupted cortical contours
- Nondisplaced: fracture line defining one or several fracture fragments; however, the external cortical contours are not significantly disrupted
- Most pediatric distal phalanx fractures are nondisplaced, with support provided by the robust periosteum.3
I - Intra-articular involvement
- Fractures that enter a joint with one or more of their fracture lines.
- Pediatric distal phalanx fractures can have fragment involvement with the DIP joint.
- If a fracture line enters a joint but does not displace the articular surface of the joint, then it is unlikely that this fracture will predispose to posttraumatic osteoarthritis. If the articular surface is separated or particularly if there is a step-off in the articular surface then the congruity of the joint will be compromised and the risk of posttraumatic osteoarthritis increases significantly.
- Pediatric fractures of the distal phalangeal condyles are intra-articular and can involve one or both condyles. Fracture patterns include lateral avulsion fractures, unicondylar or intracondylar fractures, bicondylar or transcondylar fractures, and a shearing fracture.3
C - Closed
- Closed: no associated wounds; the external environment has no connection to the fracture site or any of the fracture fragments.7-9
Pediatric distal phalanx fractures: named fractures, fractures with eponyms and other special fractures
Seymour fracture
- A “Seymour fracture” is a Salter-Harris I or II fracture of the distal phalanx physis, with concomitant avulsion of the proximal edge of the nail from the eponychial fold, flexion deformity at the fracture site, and frequently ungual subluxation. Some have suggested that a Seymour fracture can also occur in a juxta-epiphyseal position, 1-2 mm distal to the physis in the metaphysis.3,14
- These displaced fractures typically occur from crush injuries to the distal phalanx, resulting from a volar force and the dorsal apex angulation of the diaphysis compared with the epiphysis. The commonly associated nail bed laceration technically makes most of them open fractures because the nail is avulsed and the germinal matrix is torn.1,14,15 This nail bed laceration is often not visible, but because the nail plate is typically superficial to the eponychial fold. This makes the nail appear longer compared with the uninjured digits and hides the underlying nail bed laceration.1
- The distal phalanx is typically in a flexed posture as a result of the imbalance between the terminal extensor and FDP tendons. Because of this flexed posture of the distal phalanx, Seymour fractures often are misinterpreted as DIP dislocations or bony mallet injuries, but displacement in Seymour fractures occurs at the site of the physis/fracture rather than the DIP joint.1,16
- Posteroanterior radiograph views of the injured finger may appear normal. Therefore, lateral views are essential to confirm a Seymour fracture diagnosis.
Imaging
- Routine AP and lateral X-rays
Treatment
- Since these are nearly always open injuries, the optimum treatment for Seymour fractures requires early recognition and surgical management.4
- Treatment of open Seymour fractures requires surgical intervention and should consist of the following: nail removal, thorough irrigation and debridement of the fracture, gentle removal of the incarcerated nail bed from the fracture site, reduction of the fracture with or without pinning, repair of the nail bed if a substantial proximal flap exists, replacement of the nail plate underneath the eponychial fold, and splinting or casting.3 Small oblique incisions that are directed proximally toward the DIP joint at the junction of paronychial and eponychial folds may be necessary to allow eponychal fold reflection in order to provide adequately visualize and expose of the nail bed laceration.3 Hyperflexion of the digit also aids in visualization and allows for thorough irrigation and debridement of the fracture site.1 Seymour fractures are usually unstable, and reduction should therefore be maintained by K-wire fixation. Fluoroscopy is used for placement of a K-wire. K-wire fixation will cause minimal iatrogenic damage to the epiphysis.16 Postoperative parenteral antibiotics should also be administered, followed by a short course of oral antibiotics for approximately 5-7 days.3,15
- The rare case of a closed Seymour fracture can be managed with closed reduction and a splint; however, since children may not be compliant with splint wear, even these fractures are often managed surgically.1
- Fracture instability tends to occur if the nail plate is completely removed and not replaced, and the avulsed nail therefore should always be replaced. Malunion with residual pseudomallet or flexion deformity can occur in Seymour fractures treated without fixation.3
Complications
- Infection
- Osteomyelitis
- Premature physeal closure
- Nail bed deformity
- Dorsal rotation of the epiphysis
- Articular deformity
- Extensor mechanism dysfunction
- Nail growth disturbance
- Loss of DIP joint flexion
- Malunion
Outcomes
- In one study, open fractures were managed surgically with thorough debridement, nail removal, and open reduction, with K-wire fixation if necessary, and closed fractures with a splint. No infections were noted, and the fractures healed with no significant deformity at an average follow-up of 18 months.16
- In another study on 24 patients with Seymour fractures, nine had closed injuries and were treated with closed reduction and splinting using a standardized forearm-based finger splint in intrinsic-plus position. Fifteen underwent surgical management. Debridement, open reduction, nailbed repair, and splinting were performed on 9 patients. Open reduction, debridement, and K-wire fixation across the DIP joint was performed on 5 patients due to instability. After surgery, the same forearm-based splint was used to immobilize the affected digit. Clinical results revealed that 23 of the 24 patients had re-established full motion in comparison with the corresponding digit of the opposite side, with a mean motion range of 80°. No infections were reported. At the 1-year follow-up, no patients complained of pain, and patient satisfaction was primarily good or excellent.14
Mallet finger fracture
- Mallet finger fractures in children are somewhat similar to those occurring in adults, but there are several important distinctions between the two, and they consequently must be considered separately:1,14,17
- In children the terminal extensor tendon inserts on the epiphysis and the volar FDP inserts on the metaphysis.4
- The distal phalanx physis is either still open or gradually closing in pediatric patients, approximately around 13–16 years of age.18
- In adult patients, mallet finger deformities result from an injury or laceration to the extensor tendon with or without an associated fracture, but in skeletally immature children it typically occurs due to an avulsion fracture of the extensor tendon of the distal phalangeal epiphysis.1,17
- This avulsion results in an intra-articular fracture, which may extend to or through the metaphysis of the distal phalanx, resulting in a Salter-Harris type III or type IV fracture, respectively.1
- Although a Salter-Harris I or II fracture of the distal phalanx mimics the appearance of an adult mallet finger on clinical exam, it does not involve the DIP joint surface as in adults.3
- Typically, bony mallet injuries occur as a result of an axially-directed load or flexion force applied to on an extended fingertip, which drives the tip volarly faster than the extensor can relax. These injuries are particularly common in pre-teens and teenagers, and often result from sports participation.1,3
- Active ROM exam demonstrates an active extension lag. The collateral ligaments and volar plate are stable. FDP tendon function is intact with normal sensation and normal capillary refill.
- Soft tissue swelling is commonly noted over the dorsum of the DIP joint in these injuries, and the avulsed bone fragment is dorsally displaced to a varying degree.11
- In young children, delayed diagnosis of mallet finger is common, likely because of the rarity of this injury and the fact that functional impairment often is not immediately noted.17
- Bony pediatric mallet fractures can be classified into three types:
- Type I: No DIP joint subluxation
- Type II: DIP joint subluxation
- Type III: Injury to epiphysis and physis1
Imaging
- Plain anteroposterior and lateral X-ray views will usually confirm the diagnosis.
Treatment
- Limited information is available on the management of pediatric bony mallet injuries, but many surgeons treat these pediatric patients with the same management principles used for adults. Many mallet finger fractures can be treated conservatively, and the ultimate goal treatment is to achieve adequate joint stability and prevent extensor lag and swan neck deformities.1
- Conservative treatment is generally indicated for patients with bony mallet injuries that involve less than one-third of the articular surface.1
- This should include full-time splint or cast immobilization of the DIP joint in full extension for 6-8 weeks, followed by 2-4 weeks of nighttime splinting.1
- A major issue with conservatively treating mallet fractures in children is compliance with splinting, as some patients cannot maintain the splint for behavioral reasons or an improper fit. In these situations, a transarticular K-wire may need to be placed through the DIP joint and cast the hand to protect the pin from breakage.3
- Surgical management of bony mallet injuries is generally indicated when conservative treatment fails or the injury results in joint incongruence, fails to maintain cortical bony contact after attempted reduction, has persistent volar subluxation of the distal phalanx, or involves more than one-third of the articular surface.1
- Reduction of the fracture fragment or DIP subluxation is typically performed with percutaneous K-wire fixation and may involve multiple pins to reduce the fracture and the DIP joint in extension.3
- Extension block pinning can be used to percutaneously reduce and stabilize the fracture and DIP joint.1,3
- Other surgical techniques include tension band wiring, hook plating, internal suturing, pin fixation, and the use of bone anchors. If the patient is near skeletal maturity, a screw, tension band, pullout wire, or suture anchor may be used for fixation but are rarely needed.1,3
- The Ishiguro method, which involves extension block pinning in the reduced position with the DIP joint pinned in neutral, has also been proposed as an easier and less invasive procedure to treat mallet fractures when compared with other currently available operative methods.
- This method facilitates closed reduction and permits indirect anatomical reduction of the fracture, and may therefore be applied to cases of displaced pediatric mallet fractures.18
- Aggressive physical and/or occupational therapy should be considered in children who do not regain flexion appropriately after surgery.18
Complications
- Infection
- Swan neck deformity
- Postraumatic osteoarthritis
- Skin necrosis
- Nail deformity
- Loss of fixation
- Refracture
- Extensor lag
Outcomes
- In a large review of adult and pediatric mallet finger injuries and mallet fractures, outcomes were uniformly good, with surgical treatment offering no advantage over conservative treatment.3
- In another study of 17 pediatric patients who underwent operative fixation of bony mallet fractures, 12 were treated with closed reduction and extension block pinning, 2 with open reduction followed by extension block pinning, and 3 with open reduction with intrafocal pinning.
- At the follow-up, only one patient reported pain, full extension was restored in most patients, and complications were minimal.
- The authors concluded that closed reduction and extension block pinning appeared to be an effective and minimally invasive option for these injuries.18
FDP tendon avulsion fracture
- Also known as “jersey finger,” these are uncommon injuries in the pediatric population that occur from sudden hyperextension of an actively contracted FDP tendon, which avulses the tendon from its insertion.4
- Jersey finger typically occurs in young athletes, and the nickname comes from the common injury pattern in which the athlete grasps at an opponent’s jersey, and when the jersey is rapidly pulled away, the FDP tendon is avulsed from the distal phalanx because the finger is actively flexing while being hyperextended by the jersey.4,11,20
- The ring finger is the most commonly involved digit, in part because it extends slightly beyond the other digits when the hand grasps.20
- Diagnosis of jersey finger is often missed in the pediatric population due to either lack of awareness, delay in recognition, or being mistaken for a jammed or sprained finger due to the fusiform swelling in the flexor tendon sheath. Flexion of the DIP joint and isolated profundus tendon function must be tested in order to properly diagnose these injuries.4,20
Imaging
- Standard three-view radiographs of the hand should be obtained to look for associated fracture or other injuries, and a true lateral radiograph may show the avulsed fracture fragment and thus and location of the proximally displaced tendon.
- Ultrasound can also assist in diagnosing these injuries.
Treatment
- Immediate splinting of the injured finger in a comfortable position is recommended initially for jersey finger injuries diagnosed acutely. If the injury is not addressed within 7-10 days, contracture and poor outcome may result, so a timely referral is critical.20
- Surgery is generally required unless the patient is unable or unwilling to comply with postoperative therapy, or the injury is not diagnosed acutely.21
- Acute repair involves reinsertion of the FDP tendon or attached bony fragment into the volar distal phalanx. This may require repair over a dorsal button.4 A number of surgical techniques are used to treat jersey finger, including the Bunnell pull-out suture technique, suture anchor repair, and repair of the FDP tendon with incorporation of the volar plate.21
- Injuries that present 3-4 weeks after injury are considered chronic, and treatment should be guided by a combination of patient factors and technical considerations. If the DIP joint is supple, and the patient’s main concern is loss of dexterity, staged FDP reconstruction may be a reasonable option. DIP joint arthrodesis with FDP excision and FDS tenolysis may be used to treat a painful or unstable joint.21
Complications
- Contracture
- Adhesion formation
Outcome
- Since jersey finger is a zone I injury, acute repair usually has excellent results, while late reconstruction is much more complicated and outcomes are less certain.4
- Despite the inherent risks of the pull-out suture technique, excellent outcomes are obtainable when the surgical technique and post-operative rehabilitation are executed appropriately.21
Related Anatomy
- The pediatric distal phalanx consists of a distal bony tuft, a narrow diaphyseal shaft, a proximal metaphysis, and a base that articulates at the DIP joint with the middle phalanx. In developing children and adolescents, the physeal plate is located at the base of the distal phalanx, which has a dorsal and volar lip.1
- Ligaments that attach to the distal phalanx include the volar plate of the DIP joint and the radial and ulnar collateral ligaments (proper and accessory collaterals) of the DIP joint.
- Tendon attachments include the insertion of the terminal extensor tendon into the epiphysis of the distal phalanx’s dorsal lip, the insertion of the FDP into the volar proximal third of the distal phalanx at the metaphysis-diaphysis, and the insertion of the flexor pollicis longus (FPL) in the same metadiaphyseal region of the thumb distal phalanx.1,3
- The pediatric distal phalanx is further stabilized by fibrous septae in the pulp of the finger and ulnar and radial lateral interosseous ligaments between the base and tuft of the distal phalanx.
Incidence and Related injuries/conditions
- Metacarpal and phalangeal fractures account for 21% of all pediatric fractures. The phalanges are the most commonly injured bones in the hands of this population.1,11
- The annual incidence of phalangeal fractures in children/adolescents up to 19 years old has been reported as 2.7%.22
- Reports have shown that the proximal phalanx is fractured most frequently in the pediatric population, followed by the distal phalanx.5,6
- The incidence of phalangeal fractures is highest in children aged 10-14 years, which coincides with the time that most children begin playing contact sports. About two-thirds of these injuries occur in males, which is likely due to their participation in contact sports.1
- Toddlers and preschool-aged children are more likely to sustain distal tuft fractures in the home setting as a result of crush and laceration injuries.1
- One study found that the older the child, the more proximal the fracture that was sustained, with the median age for distal phalanx fractures being 9 years. This study also found that despite more patients being right-hand dominant, the distribution of phalangeal fractures was similar in both the right and left hands.2
- Salter-Harris II fractures are the most common of their type in pediatrics, accounting for 75% of all physeal fractures.20
- Subungual hematomas are a common related injury.