Fracture Nomenclature for Finger Proximal Phalanx Fracture Adult
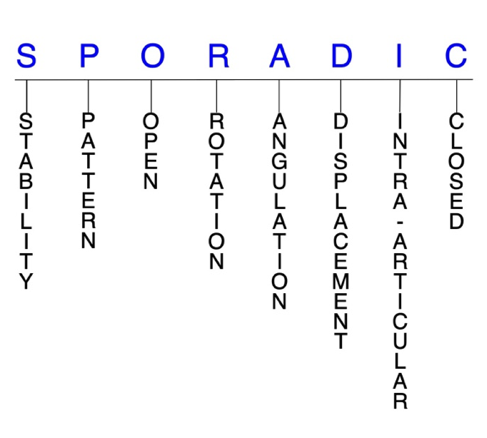
Hand Surgery Resource’s Diagnostic Guides describe fractures by the anatomical name of the fractured bone and then characterize the fracture by the Acronym:
In addition, anatomically named fractures are often also identified by specific eponyms or other special features.
For the Finger Proximal Phalanx Fracture Adult, the historical and specifically named fractures include:
Proximal Phalanx Base Volar Plate Avulsion Fracture with Complete or Partial MP Joint Dislocation
Proximal Phalanx Base MP Joint Collateral Ligament Avulsion Fracture
By selecting the name (diagnosis), you will be linked to the introduction section of this Diagnostic Guide dedicated to the selected fracture eponym.
Proximal phalanx fractures are some of the most common fractures in the body, occurring more frequently than those of the middle phalanx but less frequently than those of the distal phalanx. They often present with apex volar angulation due to the insertion of the interosseus muscle onto the proximal phalanx base, which flexes its proximal fragment while the distal fragment is hyperextended by the central slip acting on the base of the middle phalanx. These injuries can also be significantly disabling and are very difficult to treat due the presence of important joints on both ends of the bone.1-4
Definitions
- A proximal phalanx fracture is a disruption of the mechanical integrity of the proximal phalanx.
- A proximal phalanx fracture produces a discontinuity in the proximal phalanx contours that can be complete or incomplete.
- A proximal phalanx fracture is caused by a direct force that exceeds the breaking point of the bone.
Hand Surgery Resource’s Fracture Description and Characterization Acronym
SPORADIC
S – Stability; P – Pattern; O – Open; R – Rotation; A – Angulation; D – Displacement; I – Intra-articular; C – Closed
S - Stability (stable or unstable)
- Universally accepted definitions of clinical fracture stability is not well defined in the hand surgery literature. 5-7
- Stable: fracture fragment pattern is generally nondisplaced or minimally displaced. It does not require reduction, and the fracture fragments’ alignment is maintained with simple splinting. However, most definitions define a stable fracture as one that will maintain anatomical alignment after a simple closed reduction and splinting. Some authors add that stable fractures remain aligned, even when adjacent joints are put to a partial range of motion (ROM).
- Unstable: will not remain anatomically or nearly anatomically aligned after a successful closed reduction and simple splinting. Typically unstable proximal phalanx fractures have significant deformity with comminution, displacement, angulation, and/or shortening.
P - Pattern
- Proximal phalanx head: oblique, transverse, or comminuted; can involve the proximal interphalangeal (PIP) joint; these are intra-articular fractures that affect one or both condyles of the proximal phalanx head, with or without displacement; displaced fractures can affect joint congruity.
- Proximal phalanx shaft: transverse, oblique, or comminuted with or without shortening
- Proximal phalanx base: can involve the metacarpophalangeal (MCP) joint; fractures of the lateral volar base of the proximal phalanx are common and usually represent collateral ligament avulsion injuries, while comminuted fractures involving the articular surface of the base of the proximal phalanx are relatively rare.8
- Overall, spiral and oblique fractures are most common in the proximal phalanx.9
O - Open
- Open: a wound connects the external environment to the fracture site. The wound provides a pathway for bacteria to reach and infect the fracture site. As a result, there is always a risk for chronic osteomyelitis. Therefore, open fractures of the proximal phalanx require antibiotics with surgical irrigation and wound debridement.5,10,11
R - Rotation
- Proximal phalanx fracture deformity can be caused by rotation of the distal fragment on the proximal fragment. Significant malrotation can affect the position of fingertip during grip.
- Degree of malrotation of the fracture fragments can be used to describe the fracture deformity.
- Oblique fractures often produce rotational deformities, but they may also angulate or shorten.9
A - Angulation (fracture fragments in relationship to one another)
- Angulation is measured in degrees after identifying the direction of the apex of the angulation.
- Straight: no angulatory deformity
- Angulated: bent at the fracture site
- Example: displaced fractures at the base of the proximal phalanx often exhibit apex volar angulation due to the pull of extrinsic and intrinsic muscles originating in the forearm and hand, respectively.11,12
D - Displacement (Contour)
- Displaced: disrupted cortical contours (eg, bicondylar fractures of the proximal phalanx head are nearly always displaced and often comminuted).9
- Nondisplaced: fracture line(s) defining one or several fracture fragment fragments; however, the external cortical contours are not significantly disrupted
I - Intra-articular involvement
- Fractures that enter a joint with one or more of their fracture lines.
- Proximal phalanx fractures can have fragment involvement with the PIP or MCP joints.
- If a fracture line enters a joint but does not displace the articular surface of the joint, then it is unlikely that this fracture will predispose to posttraumatic osteoarthritis. If the articular surface is separated or there is a step-off in the articular surface, then the congruity of the joint will be compromised and the risk of posttraumatic osteoarthritis increases significantly.
- Fractures of the distal third of the proximal phalanx are often intra-articular and benefit from closed reduction and percutaneous pinning to minimize dissection around the PIP joint.13
C - Closed
- Closed: no associated wounds; the external environment has no connection to the fracture site or any of the fracture fragments.5-7
Proximal phalanx fractures: named fractures, fractures with eponyms and other special fractures
Proximal Phalanx Base Volar Plate Avulsion Fracture with Complete or Partial MP Joint Dislocation
- Traumatic dislocation of the MCP joint is regarded as a rare injury, but some evidence suggests that this is due to significant underreporting.14
- The capsule of the MCP joint extends from the metacarpal neck to the base of the proximal phalanx and is reinforced by ligamentous structures on all sides. The proper collateral ligaments are the primary stabilizers of the MCP joint throughout its range of motion (ROM). The volar plate stabilizes and supports the MCP joint on the palmar aspect.
- The MCP joint is weakest dorsally, as the dorsal capsule is thin and loose, with the extrinsic extensor tendons located directly dorsal to this capsule.14
- The usual mechanism of injury to an MCP joint is a fall on the outstretched hand (FOOSH), causing forcible hyperextension of the joint. Dorsal dislocations are more frequent than volar dislocations, and MCP joint dislocations are less common than IP dislocations. The index finger is most frequently involved, followed by the thumb.14
- When the MCP joint dislocates, the proximal phalanx typically moves dorsal to the metacarpal head, which can cause an avulsion fracture of the volar plate into the joint. When the interposed volar plate prevents closed reduction, the MCP dislocation is considered complex. In addition, the metacarpal head may be entrapped in the tendons and ligamentous structures as it displaces volarly.15,16
- Concomitant fractures of the base of the proximal phalanx and metacarpal head occur in about 50% of MCP joint dislocations.14
Imaging
- AP, lateral, and oblique X-ray views are needed to confirm the diagnosis. Lateral is the most useful view.
Treatment
- Some simple dislocations can be reduced non-surgically with initial MCP hyperextension followed by dorsal pressure on the proximal phalanx in conjunction with wrist flexion.
- The MCP should then be splinted for 3-4 weeks to prevent hyperextension with a hand-based MCP joint splint.14
- Complex MCP dislocations typically require open surgical reduction.16
- Simple distraction as a reduction maneuver is usually unsuccessful and can inadvertently convert a reducible dislocation into an irreducible one, as traction on the MCP joint can draw the entire volar plate dorsally so that it can be completely folded between the base of the proximal phalanx and metacarpal head.14
- Both volar and dorsal surgical approaches to MCP joint reduction have been described and utilized, with both being associated with unique advantages over the other.14,16
Complications
- Posttraumatic osteoarthritis
- Osteonecrosis
- Stiffness
- Decreased ROM
Outcomes
- Universal consensus has not yet been reached on whether a volar or dorsal surgical approach to MCP reduction is superior.16
- One study found that complex MCP joint dislocations treated on the day of injury with either a dorsal or volar approach led to good results with minimal arthritis and no functional deficits or pain.15
- In another study in which the surgical approach was determined by the surgeon’s preference, the dorsal approach was found to be faster and less likely to require a second approach to achieve reduction than the volar approach.16
- The volar approach may also present additional challenges for a surgeon less familiar with MCP joint anatomy.16
- When approaching the MP joint volarly, one may find the neurovascular bundle has been displaced into the superficial subcutaneous tissues.
Proximal Phalanx Base MP Joint Collateral Ligament Avulsion Fracture
- Fractures of the lateral volar base of the proximal phalanx are common, but rarely result in avulsion fractures of the radial or ulnar collateral ligament.8,9
- These injuries are thought to occur secondary to the pull of the collateral ligaments during forced abduction or adduction of the finger with the joint flexed.8,9
- Anatomically, the ligamentous structures of the MCP joint predispose the base of the proximal phalanx to be more vulnerable to avulsion fractures compared to the IP joints; however, PIP fractures are more common.
- The collateral ligaments of the MCP joint insert entirely on the epiphysis of the proximal phalanx, whereas in the IP joints, the insertion of the collateral ligaments includes the epiphysis and metaphysis.17
Imaging
Treatment
- Management of avulsion fractures of the base of the proximal phalanx is not as adequately covered in the literature as PIP joint avulsion fractures.17
- Small avulsion fragments comprising less than 25% of the articular surface can be treated closed, but with an element of shear stress during injury, the fragments are often larger and surgery is needed. Most commonly, a notably sized volar ulnar or volar radial fragment with a central depressed fragment of the articular surface exists.8 If there are large fragments that are significantly displaced, malrotated, or intraarticular with a step-off, then surgical treatment is indicated. Open reduction and internal fixation may also be indicated for a displaced avulsion fracture with gross instability.18 A volar A1 pulley sparing technique for fixation of MCP joint avulsion fractures is another minimally invasive and direct approach that can be used to internally fix these fractures.17,18
Complications
- Flexor tendon adhesion
- Bowstring of flexor tendons
- Plate prominence
- Stiffness
- Post-traumatic arthritis
Outcomes
- Several studies have yielded positive outcomes in patients treated with the A1 pulley sparing technique for fixation of MCP joint avulsion fractures.8,17,18
- In one study, all fractures treated with this technique healed uneventfully and anatomical reductions were regained. All patients also regained finger joint ROM and none presented with MCP joint instability. This technique allowed the fracture fragments to be reduced and fixed from the volar aspect of the finger with less risk of damage to the flexor tendon or MCP joint.18
- Another study reported satisfactory results in which all patients revealed full- or almost-full ROM of the MCP joint without evidence of lateral instability, grip strength of at least 90% of the uninjured hand, and no flexor tendon disturbance.17
Related Anatomy
- The proximal phalanx consists of a distal phalangeal head that articulates at the PIP with the middle phalanx, a narrow diaphyseal shaft, a proximal metaphysis, and a base that articulates at the MCP joint with the metacarpal.
- The ligaments associated with the proximal phalanx at the PIP and MCP joints are the joint capsule, the collateral ligaments (proper and accessory collateral), and the volar and palmar plates. The transverse and oblique bands of the retinacular ligament are also associated with the proximal phalanx. The oblique band originates on the lateral volar aspect of the proximal phalanx and attaches dorsally to the common extensor, while the transverse band originates and attaches closer to the joint line and inserts on the lateral border of the proximal phalanx.
- Tendon attachments include the sagittal bands of the extensor digitorum tendon and a flexor sheath that attaches to the sides of the proximal phalanx.
- There is a basic anatomical difference between the proximal and middle phalanges: the proximal phalanges have a longer, wider intramedullary canal with more cancellous bone, whereas the middle phalanges have a shorter, narrower intramedullary canal with more cortical bone.19 In general, fractures through cortical bone heal slower than fractures in cancellous bone.
Incidence and Related injuries/conditions
- Metacarpal and phalangeal fractures account for nearly half of all hand injuries that present to the emergency room.20
- Fractures of the proximal phalanx rank behind the distal phalanx and ahead of the middle phalanx in terms of prevalence, with on study reporting that proximal phalanx fractures account for about 13% of all hand fractures.3
- While transverse fractures tend to be more common in the middle phalanx, spiral and oblique fractures of the shaft are more common in the proximal phalanx.9
- Phalangeal fractures account for 23% of all below-elbow fractures.21