Fracture Nomenclature for Index, Long and Ring Metacarpals Fractures
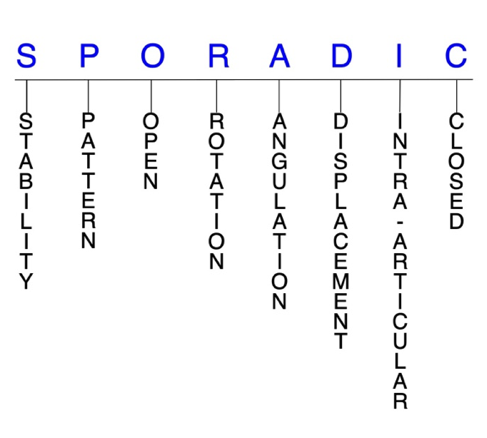
Hand Surgery Resource’s Diagnostic Guides describe fractures by the anatomical name of the fractured bone and then characterize the fracture by the Acronym:
In addition, anatomically named fractures are often also identified by specific eponyms or other special features.
For the Index, Long and Ring Metacarpals, the historical and specifically named fractures include:
Extensor carpi radialis longus avulsion fracture at the index metacarpal base
Index CMC joint dislocation and fracture-dislocation without avulsion
ECRB avulsion fracture at the long metacarpal base
Long CMC joint dislocation and fracture-dislocation without avulsion
Ring CMC joint dislocation and fracture-dislocation
By selecting the name (diagnosis), you will be linked to the introduction section of this Diagnostic Guide dedicated to the selected fracture eponym.
Fractures of the metacarpals occur less frequently than phalangeal fractures, but still represent some of the most common injuries seen in emergency departments. Reports suggest that metacarpal fractures comprise between 18-44% of all hand fractures, and about 88% of these occur in non-thumb metacarpals. The little metacarpal is the most commonly fractured of these bones, followed by the ring metacarpal, where shaft fractures also occur frequently. The incidence of index and long metacarpal fractures is similar and quite low, due in part to the rigid stability of their respective carpometacarpal (CMC) joints The neck is the most common fracture site in the metacarpals. The most typical injury mechanisms for all metacarpal fractures are accidental falls and direct blows. Most index, long, and ring metacarpal fractures are isolated, simple, closed, and stable injuries, and can be effectively managed conservatively, but surgical intervention may be necessary when closed reduction fails or is likely to fail, when associated with multiple metacarpal fractures.1-4
Definitions
- Index, long, and ring metacarpal fractures are a disruption of the mechanical integrity of these metacarpals.
- Index, long, and ring metacarpal fractures produce a discontinuity in the metacarpal contours that can be complete or incomplete.
- Index, long, and ring metacarpal fractures are caused by direct forces that exceed the breaking point of the bones.
Hand Surgery Resource’s Fracture Description and Characterization Acronym
SPORADIC
S – Stability; P – Pattern; O – Open; R – Rotation; A – Angulation; D – Displacement; I – Intra-articular; C – Closed
S - Stability (stable or unstable)
- Universally accepted definitions of clinical fracture stability is not well defined in the hand surgery literature.5-7
- Stable: fracture fragment pattern is generally nondisplaced or minimally displaced. It does not require reduction, and the fracture fragment’s alignment is maintained with simple splinting. However, most definitions define a stable fracture as one that will maintain anatomical alignment after a simple closed reduction and splinting. Some authors add that stable fractures remain aligned, even when adjacent joints are put to a partial range of motion.
- Unstable: will not remain anatomically or nearly anatomically aligned after a successful closed reduction and simple splinting. Typically unstable index, long, and ring metacarpal fractures have significant deformity with comminution, displacement, angulation, and/or shortening.
- Most metacarpal shaft fractures are inherently stable and can be treated conservatively.1
- Fractures of the border metacarpals generally tend to be less stable and more difficult to control than those of the central metacarpals. However, intra-articular metacarpal base fractures are relatively stable.1,8,9 This stability is primarily due to the osseous architecture of the CMC joints and the interosseous and dorsal and volar CMC ligaments which also provide significant stability.9 The base of the index metacarpal is the most stable of the four non-thumb metacarpals, with stability and CMC joint motion gradually decreasing towards the little metacarpal.9
P - Pattern
- Metacarpal head: oblique, transverse, or comminuted. Comminuted fractures are most common at this location.
- These fractures can involve the metacarpophalangeal (MP) joint. Although rare, these fractures appear to be more common in the index than other metacarpals. These are usually intra-articular fractures that affect one or both condyles of the metacarpal head, with or without displacement. Displaced fractures can affect joint congruity.1,2
- Metacarpal neck: most common site of fracture in the metacarpals, with the highest incidence in the ring and little metacarpals; closed metacarpal neck fractures are typically angulated with an apex dorsal position due to the deforming force of the interosseous muscles.1,2 These fractures typically result from direct axial force, causing failure of the volar cortex and flexion deformity at the fracture site.10
- Metacarpal shaft: transverse, oblique, or comminuted with or without shortening. Each fracture type presents characteristic deformities that may lead to complications if unrecognized or not managed appropriately.1,2
- In the ring metacarpal, fractures of the shaft occur most frequently, often due to punching injuries. For this reason, some consider them to be a variant of a boxer’s fracture.11
- Metacarpal base: can involve the CMC joints, and may be either intra-articular or extra-articular; intra-articular metacarpal base fractures are high-energy injuries associated with CMC dislocations, and are uncommon in the index finger, but occur more frequently in the ring and little metacarpal bases. Most extra-articular base fractures are only minimally displaced due to stability from the intermetacarpal ligaments.2
- Fractures of the ring metacarpal base typically occur with axial loading of this bone with the ring and little CMC joints flexed, causing impaction of the ring metacarpal volar base into the hamate. Fractures through this mechanism are therefore commonly associated with ring and small finger CMC joint dislocations.9
O - Open
- Open: a wound connects the external environment to the fracture site. The wound provides a pathway for bacteria to reach and infect the fracture site. As a result, there is always a risk for development of osteomyelitis. Therefore, open fractures of the index, long, and ring metacarpals require antibiotics with surgical irrigation and wound debridement.5,12,13
- Open fractures to the metacarpal head/neck area, especially those resulting from fistfights, mandate exploration to exclude involvement of the MP joint and/or extensor mechanism. After irrigation and debridement, these wounds are generally left open and internal fixation—if needed—is delayed until the wound shows no sign of infection.1,2
R - Rotation
- Index, long, and ring metacarpal fracture deformity can be caused by rotation of the distal fragment on the proximal fragment.
- Degree of malrotation of the fracture fragments can be used to describe the fracture deformity.
- Oblique and spiral metacarpal shaft fractures are usually the result of torsional forces and can cause rotational malalignment. These fractures may also angulate or shorten.1
- In contrast to angulation, rotation is poorly tolerated in metacarpal fractures, as it is magnified with flexion and often results in scissoring, which interferes with grip.4
- Fragment rotation may be difficult to appreciate on imaging, even if a fracture line is identified. Clinical exam with finger in flexion facilitates identification of malrotation.
A - Angulation (fracture fragments in relationship to one another)
- Angulation is measured in degrees after identifying the direction of the apex of the angulation.
- Straight: no angulatory deformity
- Angulated: bent at the fracture site
- The tolerable limit of angulation deformity in the neck of the index metacarpal is 15°, 20° in the long metacarpal, 30° in the ring metacarpal, and 50-70° in the little metacarpal. 2
- Malunion after a transverse metacarpal shaft fracture can also result in apex dorsal angulation in the sagittal plane, and healing of these fractures may lead to cosmetic and functional complications. 2 Metacarpal shaft dorsal open angulation interferes with function more than angulation at the neck of the metacarpal.
- The tolerable limit of angulation deformity in the shaft of the index and long metacarpals is 10° and 20-30° in the ring and little metacarpals.4
D - Displacement (Contour)
- Displaced: disrupted cortical contours
- Nondisplaced: fracture line defining one or several fracture fragment fragments; however, the external cortical contours are not significantly disrupted
- Most transverse fractures of the metacarpal shaft are minimally displaced.14
I - Intra-articular involvement
- Fractures that enter a joint with one or more of their fracture lines.
- Index, long, and ring metacarpal fractures can have fragment involvement with their respective MP or CMC joints.
- If a fracture line enters a joint but does not displace the articular surface of the joint, then it is unlikely that this fracture will predispose to posttraumatic osteoarthritis. If the articular surface is separated or there is a step-off in the articular surface, then the congruity of the joint will be compromised and the risk of posttraumatic osteoarthritis increases significantly.
- Intra-articular fractures of the metacarpal bases occur infrequently. These are high-energy injuries often concomitant with a CMC dislocation, and they occur most commonly in the ring and little metacarpals. Some have suggested that intra-articular metacarpal base fractures are underreported and underdiagnosed, due in part to the anatomic structure of the area and because of the limitation of standard x-rays when evaluating the metacarpal bases.2,9
- Differentiating between extra- and intra-articular fractures is crucial for planning an appropriate treatment protocol.2
C - Closed
- Closed: no associated wounds; the external environment has no connection to the fracture site or any of the fracture fragments.5-7
Index metacarpal fractures: named fractures, fractures with eponyms and other special fractures
Extensor carpi radialis longus avulsion fracture at the index metacarpal base
- Isolated articular fractures of the index metacarpal base—including extensor carpi radialis longus (ECRL) avulsion fractures—are believed to be rare due to the lack of motion of the index CMC joint; however, it may be a more common injury than the literature suggests, primarily because it is often missed on standard radiograph views, which do not allow the avulsion to be easily seen.1,15,16
- The mechanism of injury for ECRL avulsion fractures seems to be either axial loading of the index metacarpal—often from a punching injury—or forced hyperflexion of the hand and wrist, such as from a fall on the back of the hand with a palmar flexed wrist. In both cases, this force combines with contraction of the ECRL while the metacarpal is rigidly held in place, which avulses the ECRL at its insertion.1,15,17 The rigidity of the index metacarpal base due to its bony relations and ligamentous attachments prevents dorsal dislocation of the index CMC joint.15,17
- In some cases, an ECRL avulsion fracture may be misdiagnosed as a scaphoid injury.17
Imaging
- ECRL avulsion fractures are not easily seen on standard radiograph views, as the avulsed fragment overlies the trapezium and trapezoid and can be easily missed. A posteroanterior view with the hand adducted or a 30° anterior oblique view may allow the fragment to be more easily seen.15
- If radiographs still fail to show the injury, a bone scan or a CT scan may be necessary to detect the injury.17,18
Treatment
- Due to the rarity of ECRL avulsion fractures, there is no universal consensus regarding the optimal treatment for these injuries. There are proponents of conservative and surgical management strategies, and positive outcomes have been found with both.1,15,17,19
- Conservative treatment may include rest and immobilization with a neutral forearm cast or splint for approximately 4 weeks, followed by early mobilization.15,17 Conservative treatment may result in a small dorsal bony prominence, which can be removed if necessary.15
- Operative management is theoretically attractive, and justification for surgical reattachment includes restoration of the integrity of the ECRL, reconstitution of the articular surface of the second CMC joint, and elimination of a potentially irritating fragment of dorsal bone.1 When surgery is indicated, open reduction and internal fixation (ORIF) has been advocated as the preferred surgical intervention by most authors.19
Complications
- Post-traumatic osteoarthritis
- Metacarpal boss
- Impaired grip strength and wrist extension
- Wrist deformity
Outcomes
- Outcomes following conservative treatment for ECRL avulsion fractures have been mixed, with some studies reporting success and others revealing reduction failures or notable complications.15,16,17,20
- Surgical intervention for these injuries, primarily through ORIF, is generally associated with positive outcomes in which joint surface integrity and grip stability are restored. There has been no difference in outcomes demonstrated between non-fragment and fragment avulsions, and there is no direct comparison of surgical techniques and subsequent outcomes, but several different methods of ORIF have been successful. In most reported cases, a K-wire has been used while others used suture anchors.17,18,19
- Internal fixation has also been found to be well tolerated and may provide a more stable fixation than K-wires alone. In addition, headless screws provide excellent compression at the fracture site and may cause less soft tissue irritation.19
Index CMC joint dislocation and fracture-dislocation without avulsion
- The index CMC joint is an arthrodial diarthrosis, which is inherently stable due to the geometry of its articular surfaces, ligamentous integrity about the joint, and the tethering action of the long extrinsic wrist extensors. With the long CMC joint and distal carpal row, it forms the stable keystone of the transverse and longitudinal arches of the hand.8,21 The index CMC joint also has an intimate relationship with the ECRL and ECRB tendons, which help generate additional stability.22 As a result of its extreme stability, the index CMC joint also has very limited mobility: it only allows approximately 1-11° of motion in the flexion-extension plane.8,9,22
- Dislocations and fracture-dislocations of the index CMC joint are rare, especially when compared to equivalent injuries in the thumb and ulnar-sided digits.23 Most cases are isolated dorsal dislocations of the index CMC joint, while isolated volar fracture-dislocations are extremely rare; however, some authors state that it is difficult to understand how dislocation can occur without a fracture on account of the limited mobility of the index CMC joint.15,23 The suspected injury mechanism is hyperflexion of the hand and wrist, but some reports have found that forced hyperextension of the hand with adduction and axial shear around the index CMC can also be responsible.23,24 In some cases, dislocation and/or fracture-dislocation of other CMC joints can occur concomitantly with this injury.8
Imaging
- These injuries are often missed on routine radiograph views because they are difficult to visualize. Using images in 30° of supination with the thumb abducted may therefore be needed to observe the joint surfaces better.22,24
- CT scans may also be necessary to show the joint and bony structures in greater detail.22,23
Treatment
- It is difficult to make definitive treatment recommendations for index CMC joint dislocations and fracture-dislocations because there are no studies with an adequate number of patients to derive a strong conclusion.22
- Nonsurgical treatment consists of closed reduction, in which traction of the index finger is performed and dorsal pressure is applied on the deformity at the index metacarpal base. Immobilization should be used for 6 weeks. After removal, a physical therapy program is initiated. If there is loss of reduction or no possible reduction, surgical management is performed.22
- Various types of surgical interventions have been described for these injuries, including closed reduction and percutaneous pinning (CRPP), ORIF, open reduction and osteosynthesis with K-wires, arthrodesis, and primary fusion of the central CMC joints.22 Some authors suggest immediately performing closed reduction with K-wire fixation as the initial treatment for these injuries, which is used to maintain the reduction for 6-8 weeks. However, this may not always be possible, and open surgery is usually necessary if it is difficult to apply a closed reduction.8,22 The goal of open reduction is to restore the anatomical part that has not been established by nonsurgical treatment or closed methods.22
- For multiple CMC joint dislocations, CRPP or ORIF is nearly always indicated. The dislocated joints are well visualized through a dorsal longitudinal incision. Reduction is usually simple and can be maintained with K-wires extending from the metacarpals into the carpus.1
Complications
- Pain
- Impaired grip strength
- Deformity
- Post-traumatic joint arthritis
Outcomes
- The majority of studies on index CMC dislocations and fracture-dislocations have reported good outcomes regardless of the type of treatment performed, without report of pain or functional alterations.22
ECRB avulsion fracture at the long metacarpal base
- The rigid fixation of the long metacarpal base to its surrounding structures prevents dorsal dislocation of the long CMC joint during forced wrist hyperflexion; this is why an avulsion fracture is the more common outcome of this force, rather than a dislocation.27
- Current literature shows that isolated ECRB avulsion fractures are always accompanied with fracture of the long metacarpal base.28
Imaging
- Anteroposterior, lateral, and oblique radiograph views are usually necessary to identify the avulsed fracture fragment. Diagnosing an isolated ECRB avulsion fracture may be difficult if the injury is closed. If irregularity is seen on the X-ray at the long metacarpal base, then advanced radiographic imaging may be needed. In some cases a CT scan or MRI may be used to visualize the fragment and rule out significant soft-tissue injuries.29
Treatment
- Since ECRB avulsion fractures are so rare, consensus is lacking on the optimal management of these injuries, and both conservative and surgical approaches have been utilized.27
- Some experts claim that long metacarpal avulsions result in minimal disability, and therefore only require supportive conservative treatment.29
- Others point out that while closed reduction of these injuries can be easily obtained, it is extremely difficult or impossible to maintain with closed means. According to this reasoning, surgical management is needed for all ECRB avulsions.29 ORIF with anatomic repair of the detached tendon is conceptually and technically simple, and the associated risks are manageable when the appropriate technique is used. ORIF has been found to offer several advantages over closed treatment:
- With low-profile internal fixation, reduction is easily maintained, thus avoiding the formation of metacarpal boss. Anatomic reduction and repair of the ECRB improves grip and dorsiflexion strength.
- Open reduction and interfragmentary screw fixation allows for fracture compression, provides direct access to the tendon for repair, and avoids the complications inherent with percutaneous fixation.29
- Different surgical techniques may be used for fixation of the long metacarpal base, including tension band and K-wire fixation, screw fixation, or suture anchors.28
- Simple ECRB avulsion fractures—in which the tendon is still attached to the fragment—can be reduced by tension-band wiring or screw fixation. But when the tendon is also avulsed from the fragment, both injuries must be addressed. This is usually accomplished with screw fixation of the bony fragment and a suture anchor to reattach the ECRB.26
- After surgery, the wrist should be immobilized in a below-elbow cast with the wrist in slight extension for up to 6 weeks.25,26
- It is believed that the ECRB is the most effective wrist extensor and serves an important role as a wrist stabilizer. This is on account of a smaller moment arm for radial deviation and the availability of the entire muscle for wrist extension, since it is unaffected by elbow position. This capacity of the ECRB is commonly cited as the reason to preserve it and reattach the avulsed fragment whenever possible.30 Additionally, the reduction of the bony fragment restores the integrity of the joint surface and prevents it from abrading the finger extensor tendons, which could lead to late rupture.26
Complications
- Posttraumatic osteoarthritis
- Metacarpal boss
- Weak wrist extension strength
- Impaired grip strength
- Wrist deformity
Outcomes
- Although case series and cohort studies of ECRB avulsion fractures are lacking, case reports have shown that positive outcomes are feasible using both conservative and surgical interventions.25,26,30,31
Long CMC joint dislocation and fracture-dislocation without avulsion
- Long CMC joint dislocations are rare, primarily due to the robust stability of the joint.25,31
- The base of the long metacarpal is bordered by 3 flat articular surfaces and bound by stout volar and dorsal ligaments, making it the keystone of the transverse and longitudinal arches of the hand. The relationship between the flat articular surfaces and stout ligaments creates a rigid central pillar about which the thumb and ulnar digits move.31
- Dislocations and fracture-dislocations of the long CMC joint therefore require considerable energy and are frequently associated with concomitant injures to the other CMC joints and adjacent soft tissues.31
- The most common mechanism of injury is dorsal or volar levering of a clenched hand, such as around handlebars or in a closed fist.31
- Dorsal dislocations of the long CMC joint are more common than volar dislocations, and divergent dislocations are extremely rare.32
Imaging
- Anteroposterior, profile, and oblique views are typically taken, but long CMC dislocations and fracture-dislocations are frequently missed at initial presentation, especially when only routine radiographs are taken.8,33
- On posteroanterior radiographs, the dislocation can be suspected when loss of parallelism between CMC joints is found or when an apparent shortening of metacarpals is noticed.34
- A CT scan may be needed if radiographs fail to identify the injury.34
Treatment
- Due to insufficient evidence, treatment guidelines for long CMC dislocations are lacking. Both conservative and surgical treatment methods have been utilized for these injuries.31
- Some authors recommend initially treating long CMC dislocations diagnosed early with conservative closed reduction under procedural sedation using splint immobilization; however, this may be difficult to perform, and the approach is associated with a high risk of redislocation.32,34,35
- Given this information, most long CMC dislocations are treated surgically, especially in cases of symptomatic chronic dislocation or if there is excessive swelling or an associated fracture.31,34
- The most common surgical procedures used are ORIF and CRPP.34
- Fracture-dislocations in which closed reduction and K-wire fixation is used are often difficult to reduce because of the pull of the extensor carpi radialis tendon. If it is difficult to apply a closed reduction, open reduction should be considered.8
- In ORIF, the goal is to reconstruct the rigid central column of the hand, and joint debris and impediments to reduction such as trapped tendons need to be removed before definitive treatment begins. Transverse and oblique incisions are most often recommended for exposure of the CMC joint.31
- The method of fixation most frequently used for long CMC dislocations is multiple K-wires.31
- Some patients treated with open reduction may experience problems like residual pain at the long CMC joint and grip weakness. Arthrodesis may be needed in such cases.
- Some studies have even suggested that arthrodesis be considered as the primary treatment for certain unstable long CMC fracture-dislocations.31
- After surgery, the wrist should be immobilized for up to 6 weeks to allow fusion.
Complications
- Neurovascular injury
- Chronic CMC joint instability
- Posttraumatic osteoarthritis
- Complex regional pain syndrome
- Interosseous muscle weakness
- Impaired finger ROM
Outcomes
- Reports have been published of long CMC dislocations managed with closed reduction that have yielded good long-term results.31
- In one series of 11 dislocations of the index and long CMC joints, 1 was treated with primary CMC arthrodesis and the other 10 with reduction and K-wire fixation alone.
- There were 4 unsatisfactory results, 1 related to an ulnar nerve palsy and the other 3 related to CMC joint arthrosis, but successful fusion of the involved CMC joint provided an excellent result in 2 of these 3 patients.31
- Delayed treatment of long CMC dislocations has been found to result in poor functional outcomes and chronic residual pain.32
- Intense postoperative physiotherapy has also been associated with increased chances of achieving a satisfactory outcome.35
Ring CMC joint dislocation and fracture-dislocation
- While still generally rare, the rate of dislocation is much higher in the ring and little CMC joints than the index and long CMC joints, and concomitant hand injuries are common.36 Although isolated dislocations are possible, ring CMC joint fracture-dislocations are far more common.37
- As opposed to the first three digits, the ring CMC joint is extremely mobile due to its saddle shape anatomy and loose ligamentous attachments, which makes it more vulnerable to injury.36
- The likely mechanism of injury in ring CMC dislocations is longitudinal trauma upon a volarly flexed wrist, such as in a fistfight or from a biking accident.36,38 An indirect injury to the ring metacarpal is unlikely to lead to an isolated fracture, and when a bending or torsional stress is applied, it can lead to an associated small CMC joint dislocation.37
- Fracture-dislocations of the ring and little CMC joints are potentially more severe than those of the little CMC joint alone.39
- Strong dorsal ligaments with additional dynamic support of wrist extensors make dorsal ring CMC dislocations more common than volar ones.38
- Isolated fractures of the ring metacarpal should raise suspicion of an associated ring CMC joint dislocation, since the two injuries can occur together.1
Imaging
- Ring CMC dislocations are subtle and can be easily overlooked with routine radiographic views. Several special views are therefore recommended:
- Oblique radiographic views with the hand pronated 30° are considered mandatory.38
- A posteroanterior view may be needed to look for features that suggest joint disruption. If the diagnosis is clinically suspected, several special radiographic views have been recommended.37
- A CT scan may also be needed to visualize the dislocation and assess the hamate for fracture of the articular surface or hook.
Treatment
- Common treatment options for ring CMC dislocations included closed or open reduction followed by stabilization with K-wires, screws, or screws and plates.39
- Closed reduction and K-wire fixation is recommended for ring CMC joint dislocations that are diagnosed within 7-10 days. Diffuse edema, overlapping of metacarpal bases and interposition of ligamentous structures may cause failure of closed reduction attempts.36 Therefore, open reduction is often necessary if a fracture-dislocation is present.36
Complications
- Pain
- Infection
- Arthrosis
- Ulnar nerve injury
- Joint incongruity
- Metacarpal shortening
- Loss of range of motion
- Posttraumatic osteoarthritis
- Reduced grip strength
Outcomes
- Delayed diagnosis and treatment of ring CMC dislocations has been associated with negative outcomes and complications. Up to 43% of patients with neglected single CMC joint injuries experience residual pain and impaired function, but with appropriate management, up to 87% of patients return to full work and sporting activities with negligible pain.40
- In one study, 15 patients with ring and little CMC fracture-dislocations were treated with either CRPP or open reduction and percutaneous pinning (ORPP). Results indicated that the CRPP group experienced greater improvements in pain, function, and grip strength than the ORPP group.38
Related Anatomy for metacarpals index, long and ring.
Index metacarpal
- The index metacarpal consists of a distal head that articulates at the MP joint with the proximal phalanx, a supportive neck, a narrow diaphyseal shaft, a proximal metaphysis, and a base that articulates at the index CMC joint, primarily with the trapezoid. The base is shaped like a fork, with radial and ulnar condyles that envelop the trapezoid. The radial condyle articulates with the trapezium, while the longer ulnar condyle articulates with the base of the long metacarpal and capitate.24
- Ligamentous attachments include a deep capsular ligament on its volar surface that extends from the trapezium to the base of the index metacarpal, and a superficial ligament. On its dorsal aspect, the base of the index metacarpal has a deep capsular ligament that connects it to the trapezium and a superficial ligament that inserts on the trapezoid. Four strong interosseous ligaments attach the bases of the metacarpals, and the strongest of these is the ligament between the index and long metacarpals.9,15
- The tendons associated with the index metacarpal include the flexor carpi radialis tendon, which inserts onto its volar surface, and the ECRL tendon, which passes through a dorsal groove on the trapezoid to insert on the radial condyle of the index metacarpal.15,24
- The index CMC joint is an arthrodial diarthrosis, which is inherently stable due to the geometry of its articular surfaces, ligamentous integrity about the joint, and the tethering action of the long extrinsic wrist extensors.21
Long metacarpal
- The long metacarpal consists of a distal head that articulates at the MP joint with the proximal phalanx, a supportive neck, a narrow diaphyseal shaft, a proximal metaphysis, and a base that articulates at the long CMC joint with the distal pole of the capitate and 2 small facets of the index and ring metacarpals. The long metacarpal articulates with the capitate by means of a facet that is concave in its dorsal portion, where it covers the styloid process that projects proximally. This articulation distinguishes the long CMC joint and is considered a keystone due to its more proximal location than the carpal articulations of the other metacarpals.25,26,32
- The articulation of the ulnar base of the long metacarpal and the radial base of the ring metacarpal is secured by an interosseous ligament on the volar surface and a carpometacarpal ligament on the dorsal surface joins that the long and ring metacarpals to the capitate. There is also a transverse interosseous ligament between the long and index metacarpal, which is the strongest of the intermetacarpal ligaments.9,25
- The primary tendon associated with the long metacarpal is the ECRB tendon, which inserts on the dorsoradial aspect of its base, immediately beyond the styloid process. The ECRB has much greater involvement in wrist extension than the ECRL, and it stabilizes the wrist in extension during gripping.9,26
Ring metacarpal
- The ring metacarpal consists of a distal head that articulates at the MP joint with the proximal phalanx, a supportive neck, a narrow diaphyseal shaft, a proximal metaphysis, and a base that articulates at the ring CMC joint with the long metacarpal, little metacarpal, capitate, and hamate. The quadrilateral base is small and considerably variable, with 5 different morphologies. It can either articulate solely with the radial half of the hamate articular surface or it can articulate with both the hamate and the capitate through a smaller radial facet.9
- Ligaments associated with the ring metacarpal include an interosseous ligament on the volar surface and a carpometacarpal ligament on the dorsal surface.9
- The ring metacarpal is the only metacarpal that does not have any proximal tendon attachments to act as a deforming force when a fracture occurs. This is one of the main reasons that reports of isolated fractures of the ring metacarpal base are very rare.4,9
- The ring CMC joint has far greater ROM than the index and long CMC joints. It allows marked flexion-extension of up to 20°, radial-ulnar deviation of up to 7°, and pronation-supination of up to 27°. The motion of the ring CMC joint also must be intact to afford the full ROM to the very mobile little CMC joint, and its motion in all 3 directions is paramount for grasping and palmar cupping in normal hand functioning.9
Incidence and Related injuries/conditions
- Metacarpal and phalangeal fractures account for nearly half of all hand injuries that present to the emergency room.41
- Metacarpal fractures are less common than phalangeal fractures, but comprise between 18-44% of all hand fractures.42,43
- It is estimated that over 250,000 metacarpal fractures occur in the U.S. each year.42
- One study reported an overall incidence rate of 13.7 metacarpal fractures per 100,000 person-years, with these injuries comprising 33% of all hand fractures in the U.S.3
- Non-thumb metacarpals account for around 88% of all metacarpal fractures, with the little metacarpal being most commonly involved.42
- In one study on 400 participants, fractures of the little metacarpal accounted for 75.5% of all metacarpal fractures, followed by the ring metacarpal (16.3%), long metacarpal (4.1%), and index metacarpal (4.1%).44
- In another study on 785 participants, the little finger sustained 302 fractures, or 38% of all fractures distal to the carpal bones, which was primarily due to the high prevalence of little metacarpal fractures (11% of all hand fractures).45
- Men between the ages of 10-29 have been identified as the population with the highest incidence of metacarpal fractures, with a peak incidence between ages 10-19.3
- Punching a wall or door is by far the most commonly involved mechanism of injury for metacarpal fractures, while sporting activities—particularly football and basketball—account for the next largest portion.10
- Another study found that bicycle accidents accounted for a large proportion of metacarpal fractures across all demographics, while accidental falls were the mechanism of injury over a bimodal distribution of age groups less than 9 and older than 50 years old.3
- CMC dislocations and fracture-dislocations account for less than 1% of all hand injuries.35