Fracture Nomenclature for Scaphoid Fracture Pediatric
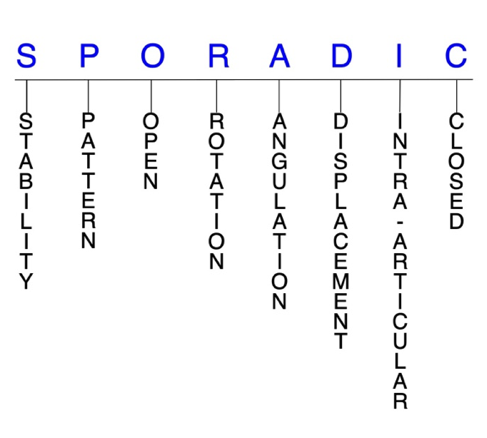
Hand Surgery Resource’s Diagnostic Guides describe fractures by the anatomical name of the fractured bone and then characterize the fracture by the Acronym:
In addition, anatomically named fractures are often also identified by specific eponyms or other special features.
For the Scaphoid Fracture Pediatric, the historical and specifically named fractures include:
Scaphocapitate fracture syndrome
By selecting the name (diagnosis), you will be linked to the introduction section of this Diagnostic Guide dedicated to the selected fracture eponym.
Carpal fractures are generally considered rare in the pediatric population. As is the case in adults, fractures of the scaphoid represent the majority of these injuries, and they account for ~0.5% of all upper limb fractures and ~3% of hand and wrist fractures in children. While common for the pediatric carpals, the incidence of scaphoid fractures is relatively low compared to adults. The usual mechanism of injury is a forced dorsiflexion wrist injury—often resulting from a fall on an outstretched hand (FOOSH)—although a direct blow or axial loading of the wrist may also be responsible. Treatment for pediatric scaphoid fractures is predominantly conservative and consists of cast immobilization; surgery is reserved for displaced fractures and patients approaching skeletal maturity.1-4
Definitions
- A pediatric scaphoid fracture is a disruption of the mechanical integrity of the scaphoid.
- A pediatric scaphoid fracture produces a discontinuity in the scaphoid contours that can be complete or incomplete.
- A pediatric scaphoid fracture is caused by a direct force that exceeds the breaking point of the bone.
Hand Surgery Resource’s Fracture Description and Characterization Acronym
SPORADIC
S – Stability; P – Pattern; O – Open; R – Rotation; A – Angulation; D – Displacement; I – Intra-articular; C – Closed
S - Stability (stable or unstable)
- Universally accepted definitions of clinical fracture stability is not well defined in the hand surgery literature.5-7
- Stable: fracture fragment pattern is generally nondisplaced or minimally displaced. It does not require reduction, and the fracture fragment’s alignment is maintained with simple splinting. However, most definitions define a stable fracture as one that will maintain anatomical alignment after a simple closed reduction and splinting. Some authors add that stable fractures remain aligned, even when adjacent joints are put to a partial range of motion (ROM).
- Unstable: will not remain anatomically or nearly anatomically aligned after a successful closed reduction and simple splinting. Typically unstable pediatric scaphoid fractures have significant deformity with comminution, displacement, angulation, and/or shortening.
- The incidence of unstable and displaced fractures of the scaphoid and other carpals is less frequent in the pediatric population because the injury etiology is typically less severe and involves fewer high-velocity mechanisms.3
P - Pattern
- Scaphoid tubercle: typically caused by direct impact with the hand in dorsifexion, ulnar deviation, and pronation, leading to a fragment avulsion by the radial collateral ligament, capsular attachments, or transverse carpal ligament8
- Scaphoid distal pole: the most common fracture location, with incidence rates ranging from 59-87% of all pediatric scaphoid fractures9 Includes transverse and avulsion fractures of the distal pole.2
- Scaphoid waist: transverse, vertical oblique, horizontal oblique, coronal, and/or comminuted; can be complete or incomplete. Less common than in the adult population: only account for ~25% of all pediatric scaphoid fractures2
- Scaphoid proximal pole: the rarest fracture location in pediatrics2 These are unstable fractures that are difficult to treat and easily missed on plain radiographs. 10,11
- The usual mechanism of injury is a forced dorsiflexion wrist injury—most commonly a FOOSH with a pronated and ulnarly deviated hand, and the wrist typically in wrist hyperextension. This causes longitudinal loading of the scaphoid and a subsequent fracture as the volar cortex fails in tension.2,10,11 Other possible injury mechanisms include a direct blow and axial loading with the wrist in neutral flexion-extension.10,11 Direct blows can also cause an impaction fracture anywhere along the length of the scaphoid, while forced dorsiflexion of the wrist typically results in a displaced distal third, waist, or proximal third scaphoid fracture.2
- Scaphoid fractures in children and adults differ in their location within the scaphoid, as most (~70%) adult scaphoid fractures occur at the waist in the middle third, while the majority of pediatric fractures occur at the distal third. Adolescents also show injury patterns that are more similar to those seen in adults.1
- A 3-part classification system based on the child’s age and presumed degree of ossification has been proposed:
- Type 1: lesions occurring in children ≤8 years in which the fracture line is purely chondral or may involve part of the ossific nucleus; these fractures are more rare and difficult to diagnose
- Type 2: osteochondral fractures in patients aged 8-11 years
- Type 3: most common type, occurring in adolescents aged ≥12 years; fractures at this age behave similar to the adult population because the scaphoid is almost completely ossified12
O - Open
- Open: a wound connects the external environment to the fracture site. The wound provides a pathway for bacteria to reach and infect the fracture site. As a result, there is always a risk for chronic osteomyelitis. Therefore, open fractures of the pediatric scaphoid require antibiotics with surgical irrigation and wound debridement.5,13,14
- Open fractures of the scaphoid may require surgical exploration to determine if articular surfaces are involved. After irrigation and debridement, these wounds are generally left open if severely contaminated and further treatment is typically delayed until the wound shows no sign of infection.15,16
- Open pediatric scaphoid fractures are also more likely to result in nonunion.17
R - Rotation
- Scaphoid fracture deformity can be caused by rotation of the distal fragment on the proximal fragment.
- Degree of malrotation of the fracture fragments can be used to describe the fracture deformity.
- Scaphocapitate fracture syndrome consists of concomitant fractures of the scaphoid and capitate with a rotation of 90-180° of the proximal fragment of the capitate. Although possible in children, this injury is extremely rare, and no cases have been documented in which the capitate fragment rotates 180°.18,19
- Opposing rotational moments on the proximal and distal poles cause dorsal angulation in scaphoid fractures.20
A - Angulation (fracture fragments in relationship to one another)
- Angulation is measured in degrees after identifying the direction of the apex of the angulation.
- Straight: no angulatory deformity
- Angulated: bent at the fracture site
- In pediatric scaphoid fractures, fracture angulation in the sagittal plane with a lateral intrascaphoid angle >45° or a height-to-length ratio >0.65 is often considered an indication for surgery.2
- Very little published information exists concerning the treatment of acute displaced carpal fractures in children.2
D - Displacement (Contour)
- Displaced: disrupted cortical contours
- Nondisplaced: fracture line defining one or several fracture fragments; however, the external cortical contours are not significantly disrupted
- Most pediatric scaphoid fractures are nondisplaced fractures of the distal pole.1
I - Intra-articular involvement
- Fractures that enter a joint with one or more of their fracture lines.
- Pediatric scaphoid fractures can have fragment involvement with the radius or any of its intercarpal joint articulations.
- If a fracture line enters a joint but does not displace the articular surface of the joint, then it is unlikely that this fracture will predispose to posttraumatic osteoarthritis. If the articular surface is separated or there is a step-off in the articular surface, then the congruity of the joint will be compromised and the risk of posttraumatic osteoarthritis increases significantly.
C - Closed
- Closed: no associated wounds; the external environment has no connection to the fracture site or any of the fracture fragments.5-7
Pediatric scaphoid fractures: named fractures, fractures with eponyms and other special fractures
Scaphocapitate fracture syndrome
- Rare but complex injury typically considered a manifestation of the perilunate injury pattern.21,22
- Consists of simultaneous fractures of the scaphoid and capitate neck with a 90-180° rotation of the proximal capitate fragment.19
- Most commonly occurs in young men between ages 20-30, and is very rarely seen and not well documented in children.23,24 In children, this injury pattern may be associated with other, more obvious fractures. It does not appear that any cases of scaphocapitate fracture syndrome have occurred in a child in which the proximal capitate fragment was rotated to 180°.19
- The most recognized mechanism of injury is a volar-applied force to a hyperextended wrist, such as from a fall from a height or vehicular accident.23
- Can be either isolated or associated with a perilunate dislocation, but a substantial force is usually required to cause a dislocation.23
Imaging
- Plain radiographs may not show the extent of the damage to the carpus. This, combined with the rarity and complexity of these injuries, may cause the diagnosis to be initially missed or incorrectly labelled as a simple scaphoid fracture.18,22 This is why a high index of clinical suspicion is needed in order to avoid misdiagnosis and ensure appropriate treatment.19,24
- If plain radiography does not lead to a satisfactory diagnosis, a CT scan may be needed, especially if a complex carpal lesion is suspected.18,23
Treatment
- The treatment of this injury pattern is controversial, particularly due to its low incidence.22
- As in adults, conservative treatment—consisting of closed reduction and cast immobilization—may be appropriate for some nondisplaced injuries, but it appears that surgery is often needed in more complex patterns.19,22,24
- Open reduction and internal fixation (ORIF) is generally considered the treatment-of-choice in children, particularly for displaced and/or comminuted fractures. A dorsal approach is most commonly used, while a volar approach is usually reserved for when decompression of the median nerve is necessary.19,24,25 K-wires or compression screws are typically recommended to achieve fixation and reduce the risk for nonunion.18,23,24 According to the literature, it is recommended that reduction of the capitate precedes reduction of the scaphoid.18
Complications
- Infection
- Avascular necrosis
- Nonunion
Outcomes
- Conservative treatment was found to elicit good outcomes in a small series of children with scaphocapitate fracture syndrome in which the capitate fracture was not displaced.19
- Literature is lacking on outcomes after surgical treatment in pediatrics, but in adults, one study in 15 patients reported that ORIF yielded better results than nonoperative treatment.26
Related Anatomy
- The scaphoid consists of a distal tubercle, a distal pole, a medial waist, and a proximal pole. It articulates distally with the trapezium and trapezoid, medially with the capitate, ulnarly with the lunate, and proximally with the radius at the scaphoid fossa. Derived from the Greek term “skaphe,” meaning skiff or boat, the scaphoid is approximately the size and shape of a medium cashew and is the largest and most radial of the proximal carpals, where it functions as a mechanical link between the proximal and distal carpal rows.10,20 In children, ossification of the scaphoid begins at an average age of 6 for boys and 4 for girls, and concludes at 15 for boys and 13 for girls. This approximately 9-year period is a time of flux in the physical nature of the scaphoid, and fractures occurring at different points behave differently depending on developmental status of the bone.2 The relatively low rate of scaphoid fractures in children may be attributed to the more cartilaginous nature of the bone during ossification, since cartilage provides a cushioning effect in the typically low-impact falls children generally encounter.4
- Ligamentous attachments of the scaphoid include the radioscaphocapitate, long radiolunate, radioscapholunate, scapholunate interosseous, dorsal radiocarpal, dorsal intercarpal, scaphotrapezium-trapezoid, scaphocapitate, and transverse carpal ligaments. The existence of several other possible ligamentous attachments, including the radial collateral and volar scaphotriquetral ligaments, is still debated.27
- The scaphoid has no tendinous insertions.
Incidence and Related injuries/conditions
- Carpal fractures are generally uncommon in the pediatric population, but the scaphoid is by far the most frequently affected of these bones. Scaphoid fractures account for ~0.45% of all upper limb fractures28 and 2.9% of hand and wrist fractures in children.29 The annual incidence of scaphoid fractures in children under age 15 is reported to be 0.6 per 10,000.28 The incidence of scaphoid fractures in pediatric and adolescent patients is believed to be rising, partially due to the growing popularity of contact sports and extreme sports like motocross, snowboarding, and skateboarding.4
- Most pediatric scaphoid fractures occur between ages 11-13. These injuries are less common in children under the age of 11, and are extremely rare at ≤8 years.4,29
Work-up Options
- Pediatric scaphoid fractures can be difficult to diagnose, as they often have subtle findings on radiographs upon initial presentation.31
- Routine and special X-rays
- The sensitivity of plain radiographs varies significantly in the pediatric literature from 21-97%, and one study found that ~13% of fractures do not appear radiographically until 1-2 weeks after injury. Therefore, these images cannot be considered reliable and tend to only be useful for confirming a fracture and following healing progression.2
- The standard radiographic evaluation of the scaphoid should consist of anteroposterior (AP), lateral, oblique, and scaphoid views.
- The scaphoid view involves placing the wrist in maximal pronation, dorsiflexion, and ulnar deviation, and is especially useful for visualizing avulsion fractures.2
- Patients with clinical symptoms of scaphoid fractures but negative radiographs should be either placed in a thumb spica short arm cast and then followed up with radiographs or advanced imaging 10-21 days later, or be evaluated with advanced imaging immediately to rule out a scaphoid fracture.10,31
- CT scan: More cost-effective, but less effective for diagnosing occult fractures than MRI. The radiation dose it delivers and lack of evidence justifying its accuracy and reliability make CT scan a less desirable advanced imaging modality for children.2,20
- MRI: Advanced imaging modality-of-choice in pediatrics for initial evaluation and follow-up of suspected fractures.2 Especially useful in diagnosing proximal pole fractures.20
- Ultrasound: May be useful, but is highly user-dependent.2
- Bone scan: May be effective for diagnosing occult fractures within 72 hours.2