Fracture Nomenclature for Hamate and Hook of Hamate Fractures
Hand Surgery Resource’s Diagnostic Guides describe fractures by the anatomical name of the fractured bone and then characterize the fracture by the Acronym:
In addition, anatomically named fractures are often also identified by specific eponyms or other special features.
For the Hamate and Hook of Hamate Fractures, the historical and specifically named fractures include:
Hamate and Hook of Hamate Fractures
By selecting the name (diagnosis), you will be linked to the introduction section of this Diagnostic Guide dedicated to the selected fracture eponym.
Fractures of the carpal bones account for ~6% of fractures overall and up to 18% of all hand fractures. The vast majority (58-89%) occurs in the scaphoid, while fractures of the other 7 carpals are uncommon and comprise ~1.1% of all fractures. The incidence of hamate fractures is not clearly defined and has been reported to be as high as 15% of all carpal fractures; however, 2-4% is a more commonly cited estimate. These fractures may occur in the body or the hamular process (hook of hamate), with the hook being fractured more frequently. Both hamate body and hook fractures are difficult to visualize radiographically and often go undiagnosed for extended periods of time, which can lead to long-term wrist dysfunction and other complications. Most nondisplaced hamate body fractures can be treated conservatively if identified at the time of injury. Surgery is typically reserved for displaced fractures and other difficult cases, but treatment for hook of hamate fractures is controversial, with some experts recommending surgery for all patients.1-8
Definitions
- A hamate fracture is a disruption of the mechanical integrityof the hamate.
- A hamate fracture produces a discontinuity in the hamate contours that can be complete or incomplete.
- A hamate fracture is caused by a direct force that exceeds the breaking point of the bone.
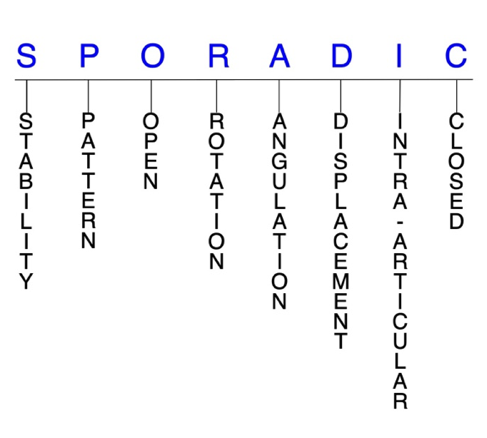
Hand Surgery Resource’s Fracture Description and Characterization Acronym
SPORADIC
S – Stability; P – Pattern; O – Open; R – Rotation; A – Angulation; D – Displacement; I – Intra-articular; C – Closed
S - Stability (stable or unstable)
- Universally accepted definitions of clinical fracture stability is not well defined in the hand surgery literature.9-11
- Stable: fracture fragment pattern is generally nondisplaced or minimally displaced. It does not require reduction, and the fracture fragment’s alignment is maintained with simple splinting. However, most definitions define a stable fracture as one that will maintain anatomical alignment after a simple closed reduction and splinting. Some authors add that stable fractures remain aligned, even when adjacent joints are put to a partial range of motion (ROM).
- Unstable: will notremain anatomically or nearly anatomically aligned after a successful closed reduction and simple splinting. Typically unstable hook of hamate fractures are very rare but painful nonunions are common. Hamate body fractures are frequently unstable secondary to the extensor carpi ulnaris (ECU) and flexor carpi ulnaris (FCU) attachments on the adjacent pisiform and the fifth metacarpal base.12This is particularly true for fractures in the coronal plane, including the so-called dorsal flake fracture, as they are frequently associated with subluxation or dislocation of the ring and little carpometacarpal (CMC) joints. Fracture-dislocations that involve >33% of the CMC articular surface are most likely to be unstable.2,5,12
P - Pattern
- Hamate hook: may occur in the distal tip, medial section, or base7 Hook of hamate fractures are typically classified as type 1.6 Fractures of the hook of hamate tip are usually avulsion fractures and have been found to account for ~11% of these injuries.13 Hook of hamate fractures of the medial third—or waist—are also rare, and account for ~13% of hook of hamate fractures.6,13 Base fractures are by far the most common, representing ~76% of hook of hamate fractures.13 Hook of hamate fractures most commonly occur in sports that involve racquets, bats, or clubs, through direct trauma or indirect mechanisms.
- During a forceful swing, the base of the racquet, bat, or club can impinge against the hook of the hamate and cause a fracture by transmitting the force of the swing through it.4
- Hamate body: may be oblique, transverse, coronal, or comminuted.3-5,14 Typically classified as type 2 and further divided into two major groups: coronal (type 2A) and transverse (type 2B) fractures
- Type 2A fractures can be further classified as dorsal oblique or splitting fractures, and these injuries are commonly associated with CMC dislocations.
- Type 2B fractures are frequently associated with axial ulnar disruptions.4,14 Others have suggested classifying hamate body fractures into the following 4 major groups: sagittal oblique fractures, dorsal coronal fractures, proximal pole fractures, and fractures of the medial tuberosity
- The position of the wrist at the moment of axial injury to the carpus partially determines the morphology of hamate body fractures in this classification system:
- With the wrist in ulnar deviation, abutment of the proximal hamate on the triquetrum results in a coronal fracture.
- When a similar axial load is applied with the wrist in radial deviation or a neutral position, the hamate fractures in the sagittal plane.
- Proximal pole fractures are typically articular osteochondral shear injuries occurring in association with complex carpal fracture-dislocations.
- Medial tuberosity fractures characteristically occur following blunt trauma to the ulnar aspect of the carpus.5
- Combined fractures involving the body and hook of hamate are rare.6
O - Open
- Open fractures of the hamate are very rare. In an open hamate fracture, a wound connects the external environment to the fracture site. The wound provides a pathway for bacteria to reach and infect the fracture site. As a result, there is always a risk for chronic osteomyelitis. Therefore, open fractures of the hamate require antibiotics with surgical irrigation and wound debridement.9,15,16
- Open fractures of the hamate may also require surgical exploration to determine if articular surfaces are involved. After irrigation and debridement, these wounds are occasionally left open and further treatment is typically delayed until the wound shows no sign of infection.17,18
R - Rotation
- Hamate fracture deformity can be caused by rotation of the distal fragment on the proximal fragment.
- Degree of malrotation of the fracture fragments can be used to describe the fracture deformity.
A - Angulation (fracture fragments in relationship to one another)
- Angulation is measured in degrees after identifying the direction of the apex of the angulation.
- Straight: no angulatory deformity
- Angulated: bent at the fracture site
- In small carpal bones like the hamate, angulation of the fracture fragments can be difficult to assess.
D - Displacement (Contour)
- Displaced: disrupted cortical contours
- Nondisplaced: fracture line defining one or several fracture fragments; however, the external cortical contours are not significantly disrupted
- In general, it has been remarked that if displacement does occur in hamate body fractures, it is not usually severe due to the presence of the strong intercarpal ligaments.5 The displacement seen in distal dorsal hamate fractures associated with CMC subluxation may require surgical attention.
- A clear definition for displacement in hook of hamate fracture has not yet been established in the literature, but according to some criteria, 30-32% of these fractures are displaced.3,20
- Due to its anatomic proximity to several ligaments, tendons, and nerves, an acute or chronically nonunited displaced hook of hamate fracture may impinge on the adjacent branch of the ulnar nerve or tendons.21
- Coronal fractures through the dorsal surface of the hamate body are often associated with subluxation or dislocation of the CMC joint caused by traction of ECU and hypothenar muscles with proximal displacement of the hamate fragment and ring and little metacarpals.2,19
I - Intra-articular involvement
- Fractures that enter a joint with one or more of their fracture lines.
- A hamate body fracture can have fragment involvement with any of its CMC or intercarpal joint articulations.
- If a fracture line enters a joint but does not displace the articular surface of the joint, then it is unlikely that this fracture will predispose to posttraumatic osteoarthritis. If the articular surface is separated or there is a step-off in the articular surface, then the congruity of the joint will be compromised and the risk of posttraumatic osteoarthritis increases significantly.
- Coronal fractures of the hamate body have also been referred to as intra-articular hamate fractures; however, these injuries are not to be confused with intra-articular fractures of the little metacarpal base.5,19 Hamate proximal pole fractures are typically articular osteochondral shear injuries that are associated with complex carpal fracture-dislocations.5
C - Closed
- Closed: no associated wounds; the external environment has no connection to the fracture site or any of the fracture fragments.9-11
Hamate fractures: named fractures, fractures with eponyms and other special fractures
Hamate dislocation and fracture-dislocation
- Hamate dislocations may occur in isolation, but are more commonly associated with other complex fractures and/or dislocations of the carpus or metacarpals.5 Isolated hamate dislocations are rare and may be volar or dorsal, and there is usually painful swelling of the hand and a bony prominence, along with shortening of the carpus on the ulnar side.22
- One of the most common fracture patterns is a hamate body fracture with a fracture-dislocation of the ring and little CMC joints, with or without ring and little metacarpal base fractures.12 These hamatometacarpal fracture-dislocations are usually sustained when a clenched fist strikes an unyielding object, and the point of impact on the two metacarpals—as well as the degree of CMC flexion during load transmission—determines the extent of CMC joint injury. The ECU tendon and hypothenar musculature are considered to be the major deforming forces.5
- Some believe that hamatometacarpalfracture-dislocations are similar enough to coronal fractures of the hamate body that the terms can be used interchangeably, while others consider them to be separate entities. Regardless of the terminology used, it appears that these injuries can be appropriately grouped together.5,19
- Hamatometacarpal fracture-dislocations are often classified into the following 3 groups:
- Type IA: subluxation or dislocation of the little CMC joint without a hamate avulsion fracture
- Type IB: identical to type IA lesions but also include a small dorsal rim hamate avulsion fracture
- Type II: subluxation or dislocation of the little CMC joint and comminution of the dorsal hamate rim
- Type III: coronal splitting fractures of the hamate body; depending on the degree and direction of displacement, these injuries may be associated with instability of the ring and little CMC joints2,5,19
Imaging
- Lateral radiographic views are helpful for showing subluxation or dislocation at the ring and little CMC joints, while oblique views are useful for identifying hamate dorsal avulsion fractures. Anteroposterior (AP) and posteroanterior (PA) views are not very effective for visualizing these injuries.1,3
- Special X-ray views, such as ulnar-deviated PA, carpal tunnel, and clenched fist views, may also be needed to properly visualize hamatometacarpal fracture-dislocations.5
- CT scans and MRIs may be used when the diagnosis remains in question or when radiographs raise suspicion for a hamate fracture.1,4,12
Treatment
- Some authors recommend conservative treatment consisting of closed reduction and immobilization for stable type IA and IB cases, especially if there does not seem to be any risk of recurrent instability after the reduction.2,5 Failure to achieve a reduction of the dislocation in these cases with the corresponding CMC joint congruence may lead to a reduction of grip strength.2
The ring and little CMC joints are quite mobile, with as much as 30° arc of flexion and extension possible at the little CMC joint and ~15° at the ring CMC. Because of this mobility and the instability associated with hamatometacarpal fracture-dislocations, surgical treatment is recommended if displacement or subluxation of the joint is evident, or when closed reduction fails.4 Surgical options include closed reduction and percutaneous pin fixation (CRPP) with K-wires, open reduction and internal fixation (ORIF), and primary excision.2,5 In types II and III injuries, ORIF is indicated to reconstruct soft tissues and restore and fix the hamate bone fragment using a plate or screws to create joint congruence. K-wires may also be considered if the stability of the CMC joint is in doubt.2
Complications
- Infection
- Impaired wrist ROM
- Reduced wrist strength
- Nonunion
- Ulnar nerve palsy
Outcomes
- Restoration of the articular surface and congruent reduction of the 2 CMC joints increases the chances of achieving an optimal functional outcome.5
- In one study in which both the ring and little CMC joints were dislocated, fixation of the coronal hamate fracture with screws and temporary bridge plate fixation of the ring CMC joint—when there was CMC instability despite hamate fixation—always led to spontaneous and stable reduction of the little CMC joint because of the ligamentous attachments, and 9 of 11 patients had full recovery.4
Related Anatomy
- The hamate is an irregularly shaped bone roughly resembling a triangle that is located in the most ulnar position of the distal carpal row. It consists of a wedge-shaped body that articulates distally with the ring and little metacarpals at their respective CMC joints, radially with the capitate, medially with the triquetrum, and proximally with the lunate, as well as a hamular process—or hook. The hook of hamate is a long, thin, curved osseous prominence located on the lower, ulnar-medial surface that projects from the hamate body into the palm in a volar fashion, 1-2 cm distal and lateral to the pisiform in the hypothenar eminence. It also contributes to the ulnar border of the carpal tunnel and the radial border of Guyon’s canal.2,4-6,8
- Ligamentous attachments of the hamate include the flexor retinaculum, which attaches to the apex of the hook of hamate, the transverse carpal ligament, pisohamate ligament, triquetrohamate ligament, and capitohamate ligament.2,23
- Tendons associated with the hamate include the flexor digiti minimi brevis and opponens digiti minimi tendons, both of which arise from the convex surface of the hook of hamate, the abductor digiti minimi tendon arising from the hook of hamate, the FCU tendon, which inserts via the pisohamate ligament onto the apex of the hook of hamate, and the flexor digitorum profundus tendon, which uses the hook of hamate as a pulley during flexion of the little finger with ulnar deviation.2,4,6,21
- Ulnar nerve and motor branch.
Incidence and Related injuries/conditions
- Fractures of the carpal bones have been found to account for 8-18% of all hand fractures24,25and ~6% of fractures overall.26
- Fractures of the proximal carpals are more common than the distal carpals, and the most commonly fractured carpal bone is the scaphoid, which represents 58-89% of all carpal fractures.24,25,27,28
- Fractures of the other 7 carpals are very rare and only account for ~1.1% of all fractures. The triquetrum ranks highest of these bones, while fractures of the remaining carpals are even less common and vary in incidence.29-31
- Most reports cite the incidence of hamate fractures—including the body and hook—as 2-4% of all carpal fractures;32,33however, it is commonly agreed that many cases of hamate fractures are missed or misdiagnosed, and their true incidence may actually be much higher, with some citing this figure to be 7%25or 15% of all carpal fractures.34
- Males are much more likely than females to sustain a hamate body fracture.14
- The specific incidence of hook of hamate fractures is also not well defined, but it is generally agreed that they occur more frequently than body fractures.7,34 The majority of hook fractures (~76%) occur at its base, followed by the medial third (~13%) and distal third (~11%).6,13 The incidence of hook of hamate fractures among professional and recreational athletes in golf, racquet sports, and baseball is much higher than in the general population.6 Only 19.4% of all hook fractures are diagnosed early and 30-32% of them are displaced.20
Work-up Options
- Routine X-rays
- Hamate fractures are generally difficult to detect on routine radiographs, but most agree that hamate body fractures are easier to visualize. However, plain radiographs have low sensitivity and specificity for hook of hamate fractures.1,3,5,7
- The main radiological characteristics of dorsal hamate body fractures include a 5-10-mm oblong fragment of bone, which projects immediately over the dorsal surface of the hamate.1,3
- This fragment is most visible on the pronation oblique and/or lateral projections and is not seen on the posteroanterior (PA) projections.1,3
- Oblique views are also important for identifying hamate dorsal avulsion fractures.12
- The degree of pronation for oblique views recommended by different investigators has ranged from 15-40°, with less obliquity showing the more radial hamate-ring metacarpal articulation.
- A lateral radiograph shows subluxation or dislocation at the ring and little CMC joints.5
- On PA radiographs, the hook of hamate overlaps with the midportion of the distal hamate body and projects as an ovoid bony density, and radiographic signs of this fracture include an absent or indistinct hook or sclerosis of the hook.6
- Disappearance of the hook on a PA view—due to congenital absence, hypoplasia, surgical resection of the hook, or erosion by amyloid tumor of the carpal tunnel—can mimic a hook of hamate fracture.3
- Special X-ray views: Ulnar-deviated PA, carpal tunnel, clenched fist, semi-supinated, and lateral with thumb abduction and radial deviation views may be helpful for assessing both hamate body and hook fractures and associated soft tissue and neural elements.5-7,12
- The carpal tunnel view cannot always be obtained in the acute phase of injury because it requires hyperextension of the wrist, which can be limited by pain and swelling.3
- Fractures at the midpoint or distal tip of the hamate hook are more readily detected in special views, whereas the more common fractures at the base are more commonly obscured.3
- CT scan: Indicated when the diagnosis remains in question, when an accurate visualization of the carpus is sought, or once radiographs raise suspicion for hamate fracture for more complete fracture characterization, since it provides the most information on the position of the fracture fragment, its possible displacement, and the amount of articular surface involved.1,3,4,12 Considered the radiographic technique-of-choice for suspected acute or chronic bony abnormalities that may suggest a hook of hamate fracture, as it is highly sensitive and specific, with an accuracy of 97.2%.6,7
- Axial 2-mm cuts through the wrist should be obtained with the hands in the prayer position. This axis is parallel to the long axis of the hook of the hamate and clearly demonstrates the fracture and its displacement, while also allowing comparison between the 2 wrists.3
- Also useful for providing information on the degree of fracture displacement.6
- MRI: An alternative to CT scans for radiographically occult pathologic conditions involving the hamate.6 MRI is less accurate than CT scans for visualizing hook cortical fractures, but superior for characterizing associated bone marrow edema, ulnar nerve injury, tendon abnormalities, and carpal tunnel abnormalities. Can be performed instead of a CT scan if the patient lacks neurologic and/or vascular competency in order to better view soft tissue structures.3
- Bone scan
- Hamate body and hook fractures are often missed or misdiagnosed as wrist sprains at emergency department presentation, which can lead to severe wrist dysfunction. This highlights the need for clinical suspicion of hamate fractures and careful evaluation of wrist injuries.4,12